Too many fail in their effort to progress activity after an injury.
You arrive at the gym feeling good but later in the day the low back soreness that has been feeling better comes back or the knee pain that seemed to be going away comes back with a vengeance after your second run. The regression happened even when the workout felt easy and pain-free at the time. Why is this happening? Why is this phase of rehab frustrating?
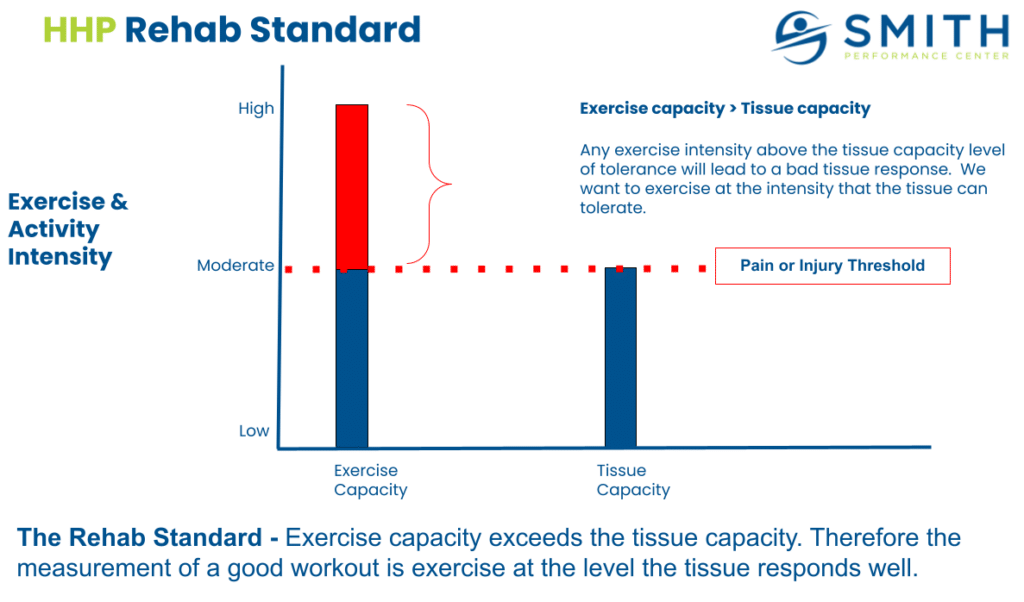
It’s due to a fundamental mistake or what we call a violation of the rehab standard, which is training at exercise capacity, not tissue capacity.
When individuals make this mistake, they start telling themselves stories like ‘I am getting too old,’ or ‘I guess I need to do something with less impact.’
However, the problem is not due to aging or the fact that the body can return to preinjury levels. The issue is also not because you didn’t warm up or stretch or any other generic advice you see on the internet. It is because you did not fully understand your problem. Rehab failures occur during activity progression because the tissue is still healing, contributors to the original injury often exist, and volume of all activity (normal daily activity and exercise) is increasing beyond what the healing tissue tolerates. And you do not have the tools to manage or modify what you are doing based off what your body is telling you.
We want to help you understand the principle of tissue capacity and exercise capacity and why it may be the reason you keep having the same setbacks.
5 Tools For Progressing Activity After Physical Therapy
There are 5 tools to use when starting to progress your activity so you do not violate the rehab standard:
- Understand your feedback loops
- Know and use your key signs before and after exercise
- Know your injury type
- Use artificial stabilization to adjust overload
- Screen for contributing factors that led to the original injury
Let’s examine each of these tools.
Understand your feedback loops
Feedback loops are crucial when starting to progress.
A feedback loop is a tool used to monitor for improvement in symptoms by determining the current baseline of symptoms, applying an action, and then reassessing the baseline of symptoms for change. The change can be better, worse, or the same. When you reassess can be directly after an action or time-based, such as an hour or a day after the action.
In the Health and Human Performance Program at SPC, a feedback loop is assessed in several ways:
- After a single action
- After an hour after the action
- After a series of actions (such as workout or a run)
- A day after the action
- After a full week of performing the new action
- After a training cycle (this is a 5 week segment at SPC)
You implement this by writing down what your symptom is. It can be numerous different tissues and each of these have different response times, so make sure you know the symptom that you do not want to experience. Prior to the activity write down what you feel.
Here is an example. You feel mild pain in your low back and slight stiffness in your low back. After the warm up including toe touches and spinning on the bike, you feel no pain but more hamstring tightness. You perform an upper body routine and the hamstring tightness reduces. You finish with the rower. In the first 5 minutes the hamstring tightness returns and starts to feel worse so you stop. An hour after the workout while sitting at the desk, the hamstring tightness worsens. By the end of the day, you feel normal again. When you wake up in the morning, your back pain feels much, much worse.
In this situation, the hamstring tightness is an important sign to build a feedback loop around the faster feedback loops. There was no pain. Low back stiffness did not return, limiting its usefulness. This would be a key sign, which will get into next.
The most important feedback loop to monitor however is the day after the action.
Know and use your key signs before and after exercise
A key sign is a tool initially used by the physical therapist during our Diagnosis and Home Plan Development Phase to determine if treatment is helping.
You can use this concept on your own. A key sign is the single, most useful tool for those who do not have pain during an activity but have pain afterward. In the example above, the hamstring tightness is a possible key sign.
This is how you can determine it for yourself. Repeat the same routine of exercises again, but substitute every activity that causes hamstring tightness with a different movement. Monitor for pain the following day, which will more than likely be gone or significantly reduced. If it is reduced, the hamstring tightness should be what you use to determine the exercises that can be done for now.
Common Key Signs for Different Injuries During Activity Progression
Low back pain:
- Discomfort or pain with Lumbar Flexion, Lumbar Extension, Sidebending Right, Sidebending Left
- Self Slump Test
- Increase in low back tightness
- Increase in hamstring tightness
- Any change in sensation
- Any change in strength
- Pain increase in normally pain free activity
- Feeling of instability (like your back feels too loose)
- Report of aching in the buttock or SI area (this is most likely coming from your back)
Neck Pain:
- Discomfort or pain with neck flexion, extension, right rotation, left rotation, right sidebending, left sidebending
- Report of tightness in the neck or upper trap
- Reporting of instability
Knee pain:
- Pain or tightness reported in the area around the knee
- Pain with knee flexion or extension
- Report of swelling or tightness in the knee
- Increased pain with lower extremity pressing movements
Know your injury type
We want you to know if you are dealing with chronic injury, recurrent injury, or an acute injury.
You may be surprised, but the definition of injury type is not consistent between providers or even the research literature. Our discussion defines them as the following:
- Chronic injury – You have had the symptoms for a long period of time. The symptoms are stable and do not seem to change much.
- Acute injury – You have had these symptoms since a recent injury and it’s the first time you have had this problem.
- Recurrent injury – You had symptoms that go away and then come back then go away then come back.
Based on the type, the issues experienced during activity progression change. A more in-depth overview can be found HERE.
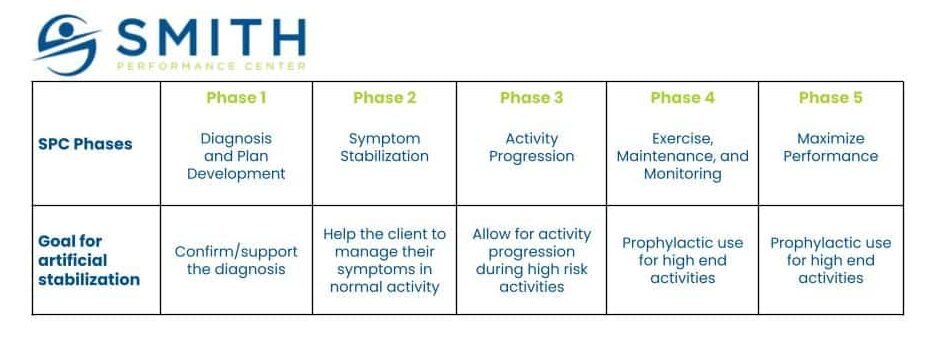
Use artificial stabilization to adjust overload
Our team uses the term artificial stabilization for any brace, tape, or externally applied product that helps you feel better during an activity.
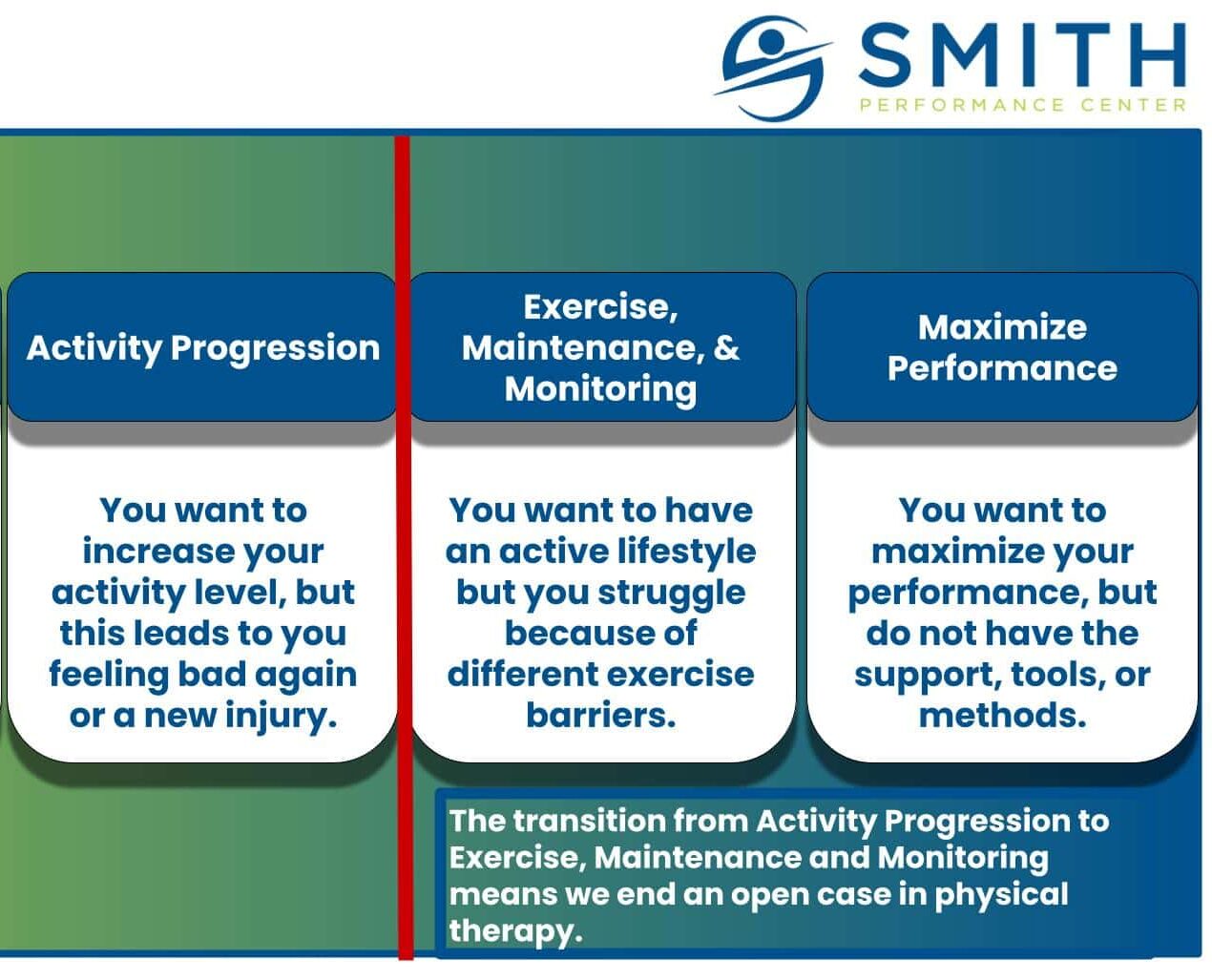
As you progress your activity, you want to rely less and less on external tools like braces or tape, but completely removing them at this stage is a mistake if they have been used significantly up to this point. However, we should not use this as you were when trying to stabilize your symptoms in the previous phase of rehab.
Individuals often fall into one of two extremes:
- Never use it with exercise.
- Always use artificial stabilization.
We see the first, never use it, often when related to the spine. There is a fear that using a lumbar brace over the spine means you no longer use the muscle. This is incorrect. You can use the brace at the times you need help or want to prevent accidental tissue overload.
The second, ‘always use artificial stabilization’, is very common around the foot in the form of orthotics. They have been convinced their foot is so problematic it can longer handle the load without the help of a custom orthotic. We believe in using it as an orthotic treatment so instead use the tools when the tissue is going to get overloaded. If you experience foot pain at 10,000 steps, use the orthotic at 8,000 steps and try to get 12,000 steps pain-free. As the foot continues to improve, increase the step count without the orthotic along with the maximum number when using the orthotic.
Screen for contributing factors that led to the original injury
Contributing factors to the original injury must be addressed during activity progression.
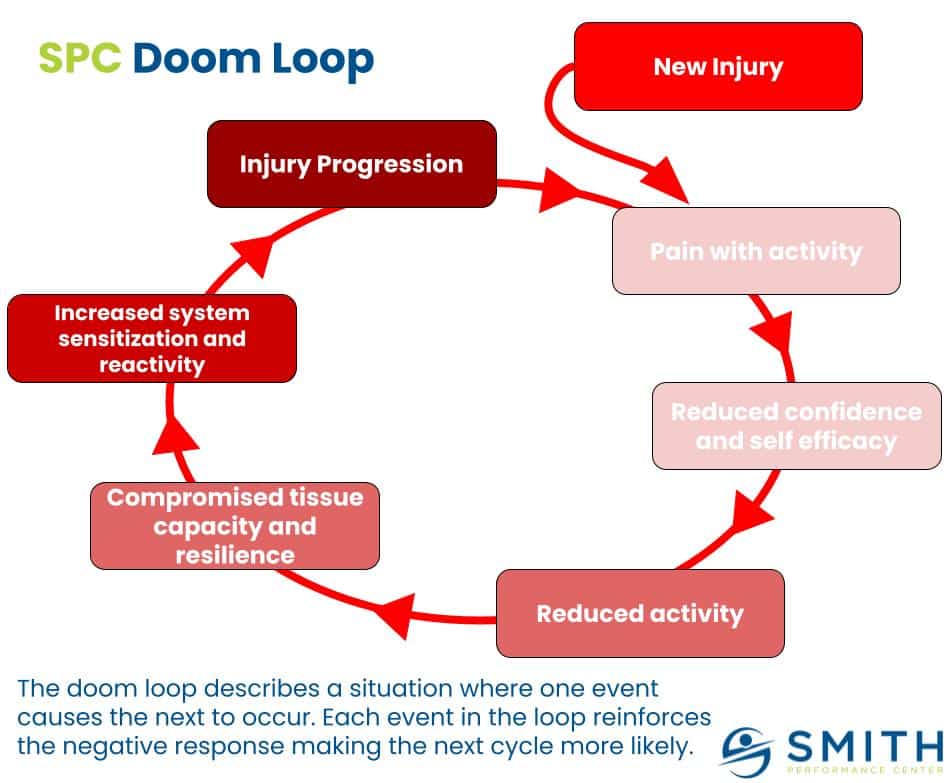
If you do not address the issues that drove you to your original injury, you will end up with the same injury again. This is a doom loop waiting to develop.
There are several contributing factors we see over and over:
- Muscle Strength
- Neuromuscular Inhibition
- Abnormal Neuromuscular Overactivation
- Balance and Proprioception
- Relative Stiffness
- Gross Motor Control
- Fundamental movements
Testing for these contributing factors can help interrupt the recurring injury cycle.
Progress your activity but respect your tissue response
The basic idea of the rehab standard is that the standard for a good workout is how your tissue responds.
It’s that simple, but actually carrying this out can be hard. Do not get discouraged by an initial bump in the road.
If you have questions or need help at this phase of your journey let us know.