When it comes to dizziness and balance issues, few areas of physical therapy are as fascinating and misunderstood as vestibular rehabilitation. In a recent conversation with Dr. Alex Griffis, PT, DPT, we discussed the most common vestibular conditions he treats, how he approaches them, and the surprising ways vision and proprioception contribute to balance.

“If the vertigo is caused by a mechanical issue, I can often resolve it quickly. If it’s more complex, we work on training the other balance systems to compensate.”
The Most Common Vestibular Issue: BPPV
According to Alex, the majority of vestibular cases he treats involve Benign Paroxysmal Positional Vertigo (BPPV). He broke down the term for clarity:
“Benign, meaning it’s not part of a life-threatening disease process. Paroxysmal, meaning it comes in fits or episodes. Positional, meaning it’s sensitive to specific positions. And vertigo, which describes the spinning sensation people experience.”
BPPV occurs when tiny calcium carbonate crystals (otoconia) dislodge and move into one of the semicircular canals of the inner ear, disrupting balance signals. Alex noted that in civilians, the posterior canal is the most commonly affected, often presenting with classic symptoms like dizziness when getting out of bed.
“People will describe it as, ‘I feel like I’m on a boat. The world is moving around me.’ It’s that false sense of motion that makes vertigo distinct from general dizziness.”
Interestingly, in veterans, Alex has seen a much higher occurrence of horizontal canal BPPV, which presents differently and often involves bizarre visual disturbances, including a phenomenon known as oscillopsia.
“Oscillopsia is when objects in your visual field appear to move or bounce, even when they are still. For example, if you’re looking at a sticky note on the wall and it appears to wiggle, that’s oscillopsia.”
This can be disorienting for patients and is a hallmark symptom of horizontal canal involvement. Alex explained that in veterans, this type of BPPV is surprisingly common, though the reason for its higher prevalence remains unclear.
The Complexity of Vestibular Cases
While BPPV is highly treatable, Alex emphasized that not all vestibular cases are the same. Some involve infections (vestibular neuritis), while others stem from degenerative conditions. These cases often require referral to specialists.
However, when vestibular dysfunction is treatable within physical therapy, Alex applies a range of techniques to help patients regain balance and control over their symptoms. One of the most intriguing approaches he described is using habituation training:
“If I can get rid of the issue entirely, that’s ideal. But if not, I’ll use habituation—meaning I intentionally provoke the dizziness to get the patient used to it. It’s like if I keep tapping your arm for an hour, eventually, you won’t notice it anymore.”
The Role of Vision and Proprioception in Balance
Vestibular function doesn’t operate in isolation. Balance relies on a tripod of systems:
- The vestibular system (inner ear)
- The visual system
- The proprioceptive system (sensory feedback from muscles and joints)
Alex shared an unexpected observation from his clinical experience:
“During the pandemic, I noticed people falling more often because they were wearing masks and couldn’t see their feet. They had no idea where they were in space. When I had them take their masks off, their balance improved.”
This highlights how visually dominant many people are when it comes to balance. He also noted that proprioceptive deficits, such as those caused by neuropathy, can make vestibular recovery more challenging.
Addressing Vestibular Dysfunction at SPC
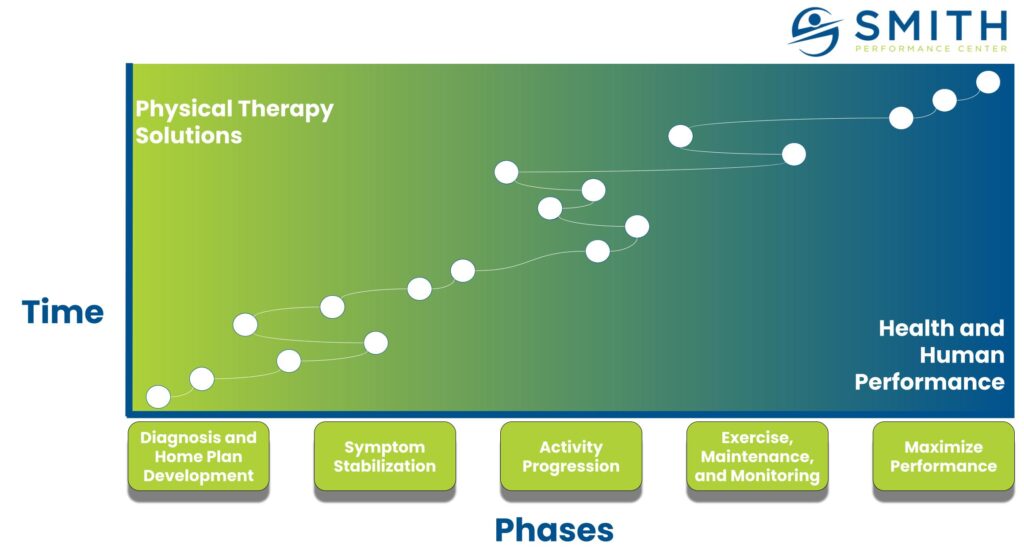
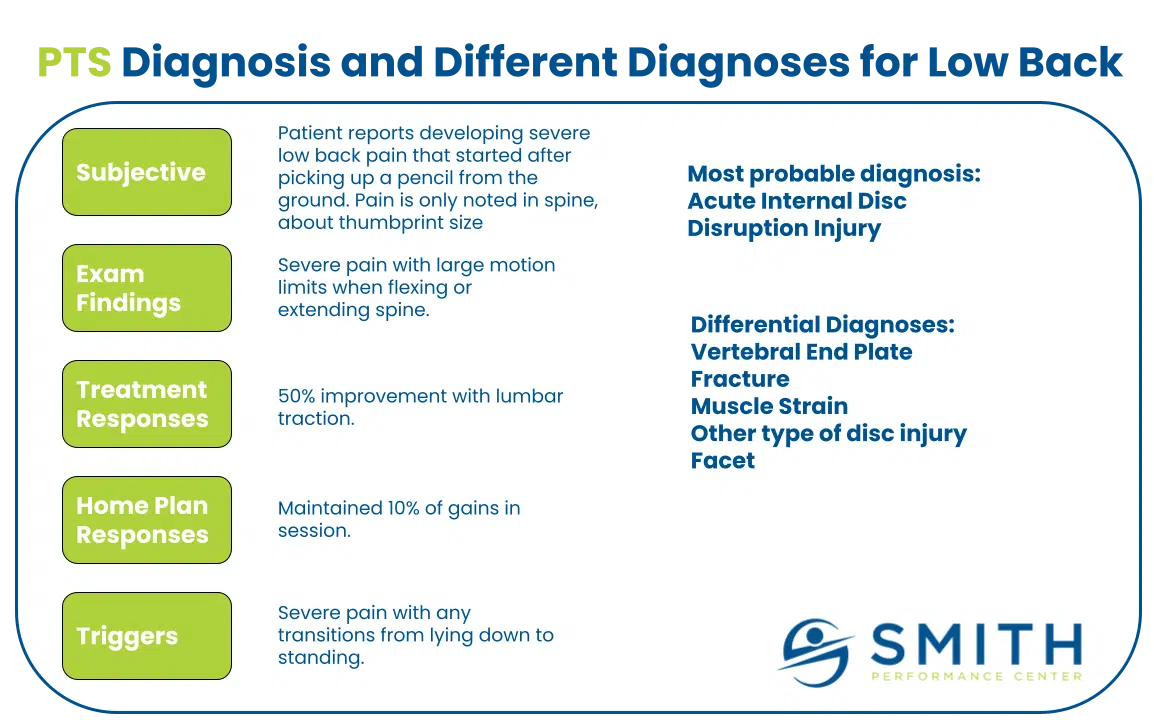
At Smith Performance Center, vestibular issues are tackled with a multi-layered approach. The process aligns with SPC’s structured phases of care. In Phase 1: Diagnostics and Home Plan Development, Alex focuses on getting the diagnosis right—determining whether the problem is rooted in the vestibular system itself or if vision and proprioception are also contributing. Once the diagnosis is clear, in Phase 2: Symptom Stabilization, the emphasis shifts to ensuring the patient can handle the treatment themselves, integrating a mix of positional maneuvers (for BPPV), habituation exercises, and balance training to restore function and build independence in managing symptoms.
“If the vertigo is caused by a mechanical issue, I can often resolve it quickly. If it’s more complex, we work on training the other balance systems to compensate.”
“After making symptoms better, we teach you how to do it on your own.”
What’s Next?
If you’ve been struggling with dizziness, unexplained falls, or balance problems, reach out to Smith Performance Center to see how we can help. Pain and loss of function can interact with vestibular issues, making movement more difficult and increasing fear of falling. At SPC, we address not only the mechanical issue but also other aspects of balance that contribute to movement limitations, helping you regain confidence and control.