
Case Study: The Dancer With Recurrent Big Toe Pain
A former college dancer came into the clinic frustrated.
She’d stopped dancing years ago, but every time she returned to even basic classes, her big-toe pain spiked. She tolerated hiking in her stiff boots, a little pain but nothing that stopped her — yet one night of dancing, and she’d hobble for a week with a throbbing big toe.
Her frustration was visible, and the best advice she’d heard—stop dancing—wasn’t one she wanted to follow. Her last visit with a podiatrist ended with an injection that helped for about a week before the pain returned. She started to believe her big toe would never handle the way she moved in college.
There didn’t seem to be a path forward.
Her experience—the fake improvement with time off, followed by a big flare when she tries to get back to what she loves—mirrors what many feel. Without understanding why and how the toe, which normally handles incredible stress, becomes so painful and fragile—and which activities trigger massive symptoms—people end up cycling through orthotics, injections, even surgery, hoping something sticks. When that doesn’t work, life reorganizes around avoiding the big toe, and the things that made life enjoyable disappear.
Getting out of this hole requires a process, not a one-off treatment.
We have to (1) diagnose the actual problem, (2) build what we call a therapeutic gap, and (3) grow tissue capacity.
In the next section, you’ll see why the toe becomes a common site for chronic injury—how the forefoot rocker and toe rocker load the joint—and why timing errors and recurrent triggers keep pain coming back.
Why the Big Toe Is a Common Injury Site
The foot is a complex system — flexible during early stance when it lands, yet rigid and powerful during push-off. It integrates 26 bones, multiple axes of motion, and large forces with every step, all while maintaining balance and forward propulsion (D’Août, 2008).
A keystone of this system is the big toe, or hallux. Its joint — the first metatarsophalangeal (1st MTP) — must stay mobile enough for propulsion yet stable enough to bear most of the forefoot load. When that balance tips too far toward either mobility or stability, it becomes a trigger-management nightmare.
Consider these forces:
During late stance and push-off, the 1st MTP experiences 1.5–2× body-weight load under the metatarsal heads (Telfer 2015).
The flexor hallucis longus (FHL) — the long toe flexor that isometrically stabilizes the big toe — becomes increasingly active as walking speed rises (Péter 2015), managing those loads across multiple joints.
This finely tuned system relies on timing. The FHL’s ability to manage tension depends on the rest of the kinetic chain. Hypermobility, or poor force absorption from the posterior tibialis, quadriceps, or glutes, can all compromise how the FHL loads. In other words, the big toe isn’t passive during gait, nor is it the strongest structure on its own — it’s an active participant in the forefoot rocker, working within a much larger system that allows efficient walking and running.
Read more about When and Where You Feel Foot Pain During Walking Is Key for Diagnosis.
Two main factors drive the big-toe injury cycle: its interdependence with the rest of the kinetic chain and its mechanical ceiling.
When stiffness or weakness higher in the chain — such as ankle dorsiflexion loss, quadriceps inhibition, or hip-extension limits — alters timing, stress at the big toe can rise dramatically. Even small tissue irritations then become persistent injuries that fail to heal because the system drives the problem.
This interdependence gives the system its power — but also its weakness. Because the 1st MTP already operates near its mechanical ceiling, even small insults can push it past its limit. A stubbed toe, an awkward step, or a jam into the front of a shoe can change how much load can be tolerated at the big toe and results in discoordination of the entire system.
Once that coordination is lost, every step becomes a replay of the same micro-irritation. The hallux never truly rests; it keeps taking load, thousands of times per day, before the tissue has healed. A small event that should have resolved becomes a chronic overload problem that now reacts to even mild activity.
This is why people often describe their toe pain as “coming out of nowhere.”
It didn’t — it’s the result of a system that was already running close to its limit, pushed past threshold by a single trigger.
Looking back at our case study, that tolerable hiking pain set her up perfectly for the sharp flare-ups that followed dancing.
When the body can’t share load effectively, the big toe becomes the bottleneck — taking the hit for the entire leg.
Because the aggravating motion repeats with every step, recovery becomes a daily battle.
The Main Diagnoses Behind Big Toe Pain
The first step in any rehab plan is getting a firm diagnosis — identifying which structure is involved, how it’s functioning, how it responds to treatment, and what triggers symptoms.
Because several structures converge at the big toe, accurate diagnosis depends on understanding when in gait the pain occurs and what kind of sensation it produces.
Read more about our diagnostic process How to Find the Real Cause of Pain: Our 4-Pillar Diagnosis Process
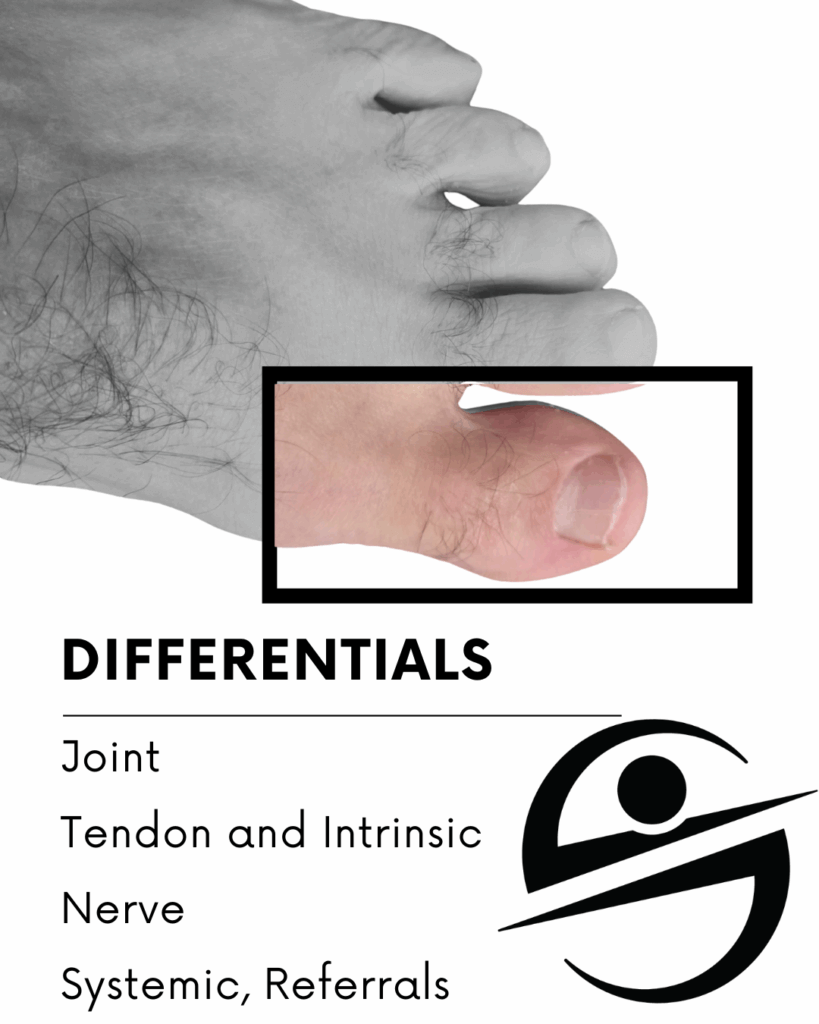
We can group these diagnoses into four broad categories — joint, tendon, nerve, and systemic/referral.
Big-toe pain can arise from several overlapping sources. Grouping them by primary tissue type helps narrow down the true problem.
Joint-Related Causes
Hallux Rigidus (Activated Arthrosis):
This is where a degenerative joint meets an inflammatory spark. We call it an activated arthrosis because it often “activates” (inflames) after repetitive stress or overload when the joint is already compromised.
Pain is typically on the top of the toe, especially at end-range extension during push-off, but it can become much more painful due to hyperalgesia (sensitization), leading to pain over the entire toe with even small movements.
This is typically a long-standing injury, and there may have been an original event years or decades in the past — sometimes called a secondary arthrosis.
Hallux Traumatic Synovitis:
Typically occurs after an acute overload event at the 1st MTP joint. This is irritation to a healthy joint, meaning imaging will often be normal on X-ray. Loading along with end-range position can be very painful.
The end ranges are often reduced compared to the opposite big toe because the synovium that lines the capsule is sensitive to stretch — more irritation means more motion loss.
This one can mimic hallux rigidus but often responds much faster. Poor management turns this into a much bigger problem.
Dorsal Bony Impingement:
A bony prominence or spur blocks motion, causing pinching pain on top of the joint.
In this situation, the joint isn’t the issue — it’s the impingement between the metatarsal and the proximal phalanx. If you pull on the big toe and move into full extension, the pain may disappear, whereas true joint pain will still hurt quite a bit.
Tendon and Intrinsic Causes
Distal Flexor Hallucis Longus (FHL) Tendinopathy:
Deep pain under the big toe or arch, worse with forefoot rocker or resisted toe flexion. EMG work confirms that this muscle is active and under increasing tension during propulsion (Péter et al., 2015).
This can also be painful under the 1st MTP during midstance, or when all of your weight is on a single leg.
Look for more pain with load, less pain with range of motion.
Flexor Hallucis Brevis (FHB) Tendinopathy:
Aching pain at the ball of the foot beneath the big toe, often described as a “stone bruise.” Usually tied to intrinsic weakness and overload at the forefoot.
Many cases labeled “sesamoiditis” fit into one of these tendon categories depending on depth and presentation.
The action of the FHB is to support the FHL. Pain in the muscle bellies of the FHB often clues you in to this smaller muscle being the primary source — though it’s not uncommon to have both involved at the same time.
Nerve-Related Causes
Not all big-toe pain is mechanical. Nerve irritation can mimic joint or tendon pain, and it’s often compounded by a second irritation elsewhere — a “double-crush” pattern.
For nerve injuries, it’s common to have both a local irritation and a secondary compression along the pathway, such as from the low back or tarsal tunnel.
Deep Peroneal Nerve Irritation:
Dorsal pain or tingling between the first and second toes, aggravated by tight shoes or excessive dorsiflexion.
Plantar Digital Nerve Irritation:
Burning or numbness under the toe during push-off. Feels like tendon pain but includes a tingling or electric quality.
Location matters, along with the quality of the symptom. If you have tingling, burning, a slight off feeling, or less perception of pressure or touch, a nerve may be involved — either as the main pain driver or secondarily sensitized by local swelling.
Systemic, Referral, or Other Causes
Finally, some conditions mimic local injury but actually originate elsewhere in the body or from metabolic issues.
Gout (Crystal Arthropathy):
Rapid onset of swelling, warmth, and redness at the 1st MTP, often mistaken for mechanical arthrosis. Look for clues like sudden onset without clear cause.
Tests for elevated uric acid can confirm gout — indicating the problem is metabolic rather than mechanical and may require medical management in addition to rehab.
Ingrown Nail or Infection:
Sharp, localized, and rapidly worsening pain at the nail margin or tip. There is typically redness and possible discharge from the infection, with pain centered where the redness is most visible.
Low Back Referral:
Pain can refer into the foot and big toe from the back. It’s critical during your exam to test whether movements of the spine reproduce the foot symptoms.
Multiple Pain Generators
When I get this specific about what’s causing your pain, I don’t want you to forget that it’s common to have multiple structures contributing at the same time.
This happens because the body instinctively tries to compensate and unload the originally injured tissue, often overloading the surrounding stabilizers.
For example, you may start with a jammed MTP joint (traumatic synovitis) and then develop an FHL tendinopathy, which causes local inflammation that interacts with a plantar digital nerve.
Pulling apart each issue requires a clear understanding of foot mechanics and integrating functional movement, treatment responses, and trigger management.
It is common to get pain in other areas of the foot as well while dealing with big toe pain. Read more about another commonly misdiagnosed problem: 7 Signs Your Heel Pain Isn’t Plantar Fasciitis (and What’s Really Causing It)
The Key Takeaway for Big Toe Pain
Accurate diagnosis matters because the right plan depends on what’s driving the pain.
Mislabeling a tendon or nerve problem as “arthritis” or “plantar fasciitis” or missing that there are multiple pain generators can send you down the wrong path — delaying recovery by months or ever.
Have Ongoing Toe Pain?
If your big toe keeps flaring up—even after rest or orthotics—you’re not alone. At Smith Performance Center, we specialize in understanding the why behind recurring injuries.
Schedule an Assessment to learn what’s driving your pain and how to manage it for good.
References
Péter, A., et al. (2015). EMG and force production of the flexor hallucis longus muscle in isometric plantarflexion and the push-off phase of walking. Journal of Electromyography and Kinesiology, 25(4), 621-627. https://pubmed.ncbi.nlm.nih.gov/26100463/
Telfer, S., et al. (2015). Metatarsal loading during gait: A musculoskeletal analysis. Journal of Biomechanical Engineering, 138(3), 034503. https://asmedigitalcollection.asme.org/biomechanical/article/138/3/034503/370474
Zhang, X., et al. (2022). Influence of shod and barefoot running on the in vivo first metatarsophalangeal joint kinematics. Frontiers in Bioengineering and Biotechnology, 10, 892760. https://pmc.ncbi.nlm.nih.gov/articles/PMC9148976/

