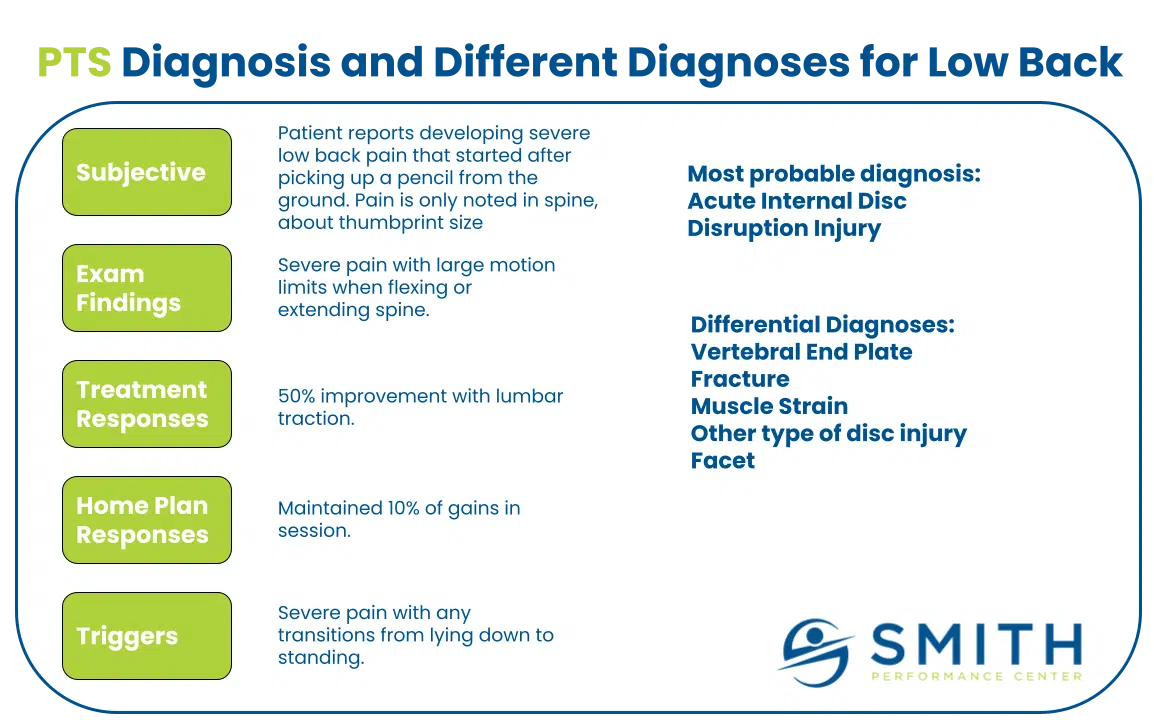
If you are trying to find the cause of pain that keeps returning, you are not alone. Many people are given quick labels like tendonitis or a pinched nerve and told to rest but that often does not solve the real issue. At Smith Performance Center, we go deeper than a label. We use a system called the 4 Pillars of Diagnosis to understand the real problem and build a clear path to recovery.

Each pillar gives us critical information about what is causing your symptoms, how your body is functioning, what helps, and what triggers setbacks. It is the difference between a guess and a plan that works.
1. Structural Diagnosis: What Might Be Injured?
This is the traditional starting point in most evaluations. We identify what structure might be involved—whether it is a tendon, joint, ligament, nerve, or muscle.
We use hands-on testing, functional movements, and your medical history to build a working theory. But naming a structure is not enough. Labels like “rotator cuff strain” or “plantar fasciitis” are just one part of the equation.
Example: If you come in with heel pain, many clinics assume plantar fasciitis. But if our testing reveals the problem is the flexor digitorum brevis, a deep foot muscle, we take a different, more effective approach.
Pro-tip: Imaging can help, but only if it matches our physical findings. MRIs and X-rays often show abnormalities that are not actually causing your pain. These false-positives are common, even in people without symptoms. One large study found that 37 percent of people in their 20s and 96 percent of people in their 80s had disc degeneration on MRI despite having no back pain. This is why we do not rely on imaging alone. We interpret it alongside your movement, physical exam, and real-life symptom patterns (Brinjikji et al., Spine, 2015).
2. Functional Diagnosis: What Is Not Working Properly?
Next, we evaluate how you move. We are not just interested in what hurts—we want to know what movement pattern is breaking down. Are you compensating? Are certain muscles not firing when they should? Is control missing?
This includes walking, squatting, lifting, or sport-specific motions. We use this information to understand how dysfunction might be overloading your body or keeping you from healing.
Why this matters: Pain often comes from poor movement, not just injury. You may feel pain in your calf, but the true issue may be a weak or underused hip. Fixing function is key to long-term resolution.
For more on how we evaluate movement, see our article on foot pain during walking.
3. Treatment Response: What Changes Your Symptoms Right Now?
Once we have a working diagnosis, we test it in real time. We apply hands-on techniques, targeted exercises, or movement corrections and immediately observe your body’s response.
If pain improves, movement becomes easier, or a key sign gets better, we know we are on the right track. If not, we reassess. This is a critical step in confirming what is really going on.
We call this the treatment hierarchy. Every injury can respond differently from person to person. There is no one-size-fits-all fix. Knowing how your body reacts helps us make better decisions and build a customized plan.
4. Trigger Management: What Makes It Better or Worse?
Pain rarely happens randomly. There are patterns – what you do, how long you do it, when symptoms appear-that give us valuable clues.
We want to know what aggravates your symptoms and what helps relieve them. Do you feel worse in the morning? After long walks? When you sit too long?
There are patterns: what you do, how long you do it, and when symptoms appear. These patterns give us valuable clues. By mapping these patterns, we teach you how to adjust activity, avoid setbacks, and gradually build capacity. You do not need to stop everything. You need a strategy.
This is where you take back control. You will learn how to identify triggers, manage flare-ups, and stay on track without guessing or waiting for the next appointment..
Why This Matters When Trying To Find The Cause Of Pain
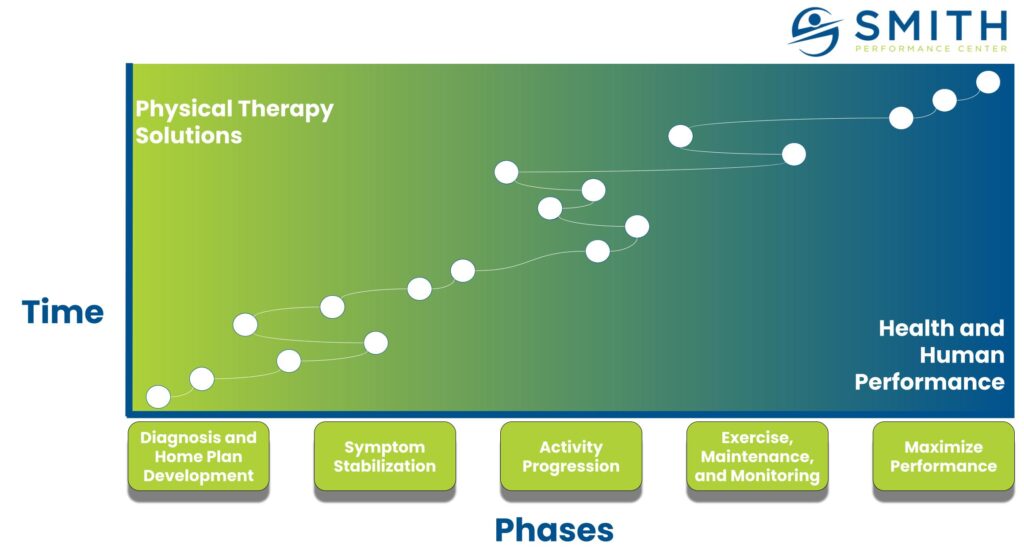
When all four pillars are considered, your diagnosis becomes more than a label. It becomes a foundation you can build on. You do not just gain clarity. You gain confidence.
Confidence that you are not guessing. Confidence that your treatment is based on real patterns. Confidence that your pain has context, and that your next steps are not just arbitrary exercises or posture corrections from a generic template.
This is where rehab starts to matter.
You do not need to stretch a tight muscle or strengthen a weak one unless the exam shows that muscle is truly involved. You do not need perfect posture if your functional exam shows that extension-based positions consistently make your symptoms worse. You do not need to activate your glutes unless there is a task where they are clearly not contributing.
At Smith Performance Center, we do not prescribe exercises to check a box. We build a plan based on validated signs, whether structural findings, functional limitations, treatment responses, or consistent triggers. Each pillar gives us a different type of signal.
Some patients have clarity in all four areas. Others may only have one. That is enough. A single validated response gives us an anchor point. From there, we test the plan, track progress, and refine based on what your body shows us.
This is how we move from uncertainty to direction. It is how rehab becomes a structured solution instead of a guessing game.
Ready to Start?
If you are tired of generic advice and temporary relief, we are here to help. Book an assessment with our physical therapy team and find the real cause of pain using our 4 Pillars of Diagnosis.