The majority of our patients have been treated somewhere else first without improvement.
When we review their case, similar process mistakes happen over and over again. Lack of diagnosis (Mistake #1) or telling a patient to just stop the activity that hurts (Mistake #4) leads to more problems and eventually to a life of inactivity. Our passion as a company is to keep moving for a lifetime and the number one reason people stop or don’t even start an active lifestyle is pain and injury. Understanding these common mistakes can help you become a better consumer of rehab services and get better faster with longer-lasting results.
The end result is the ability to do the day you want.
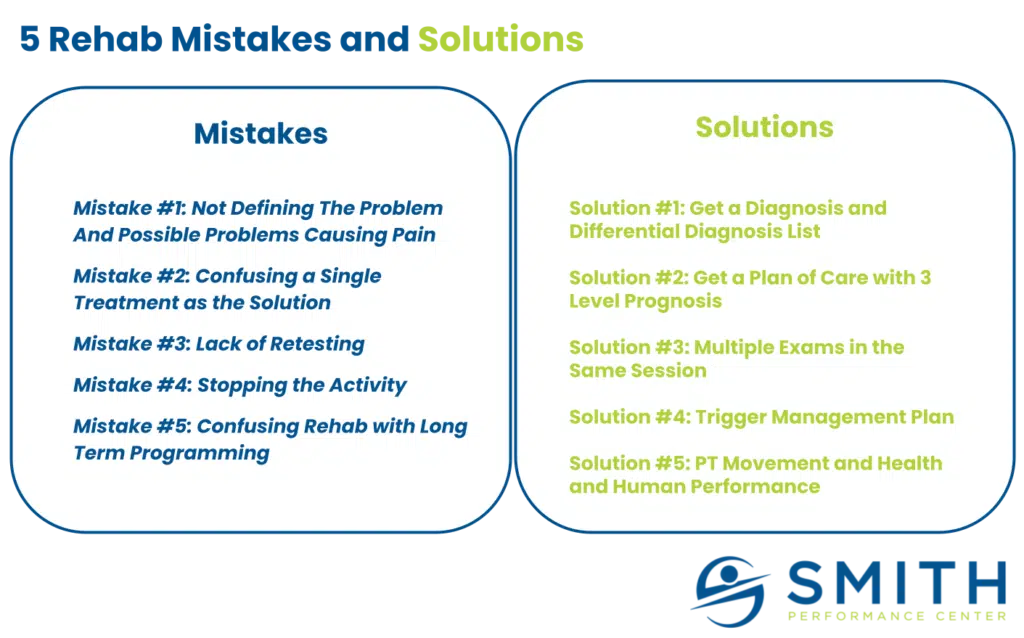
The 5 rehab mistakes and their solutions
The mistakes below are strategic errors:
- Mistake #1: Not Defining The Problem And Possible Problems Causing Pain
- Mistake #2: Confusing a Single Treatment as the Solution
- Mistake #3: Lack of Retesting
- Mistake #4: Stopping the Activity
- Mistake #5: Confusing Rehab with Long Term Programming (also known as the endless home exercise list)
The solutions allow for better strategic decisions and can be used by you and your provider:
- Solution #1: Get a Diagnosis and Differential Diagnosis List
- Solution #2: Get a Plan of Care with a Supported Process
- Solution #3: Multiple Exams in the Same Session
- Solution #4: Trigger Management Plan
- Solution #5: Exercise Program
Let’s dive into the mistakes and solutions.
5 Rehab Mistakes and the Solutions
Mistake #1: Not Defining The Problem And Possible Problems Causing Pain
A diagnosis is a crucial first step in the rehab process.
Imagine you have heel pain, a common injury that we see that does not normally have a diagnosis. The following is a list of possible tissues that could cause the pain:
- Flexor Digitorum Brevis
- Abductor Hallucis
- Abductor Digiti Minimi
- Fat Pad Trauma or Atrophy
- Calcaneal stress fracture
- Lateral Plantar Nerve
- Medial Plantar Nerve
- Tarsal Tunnel Syndrome
- Low back referral
- Hip joint referral
- Plantar Fascia
- Surgical Scars
Each of these structures requires different treatment methods. Without knowing the problem, or what we call the pain generator, then we cannot be sure the painful tissue is getting targeted.
(If you have been told that you have plantar fasciitis and you want to know more about what could be causing your heel pain, read our post ‘7 Signs Your Heel Pain Is Not Coming From Your Plantar Fascia.’)
Solution #1: Get a Diagnosis and Differential Diagnosis List
While this seems simple, the majority of patients do not get a diagnosis or a differential diagnosis list from their provider.
When we ask the patient with back pain, they typically say they were diagnosed with a slipped disc or ‘back pain’. But this is not a diagnosis and it causes significant problems in your rehab process. Without a working diagnosis, how do you create a plan? Without a working diagnosis, how do you know if you should expect improvement within a week? Without a working diagnosis, how do you know what type of treatments to perform? How do you know if the plan is working? Without a differential diagnosis list, how do you pivot to a new plan if the current one is not working?
The answer is you do not know.
This leads to a failed plan and eventually, either you or the provider gets frustrated.
(If you want to read more about how to come up with a diagnosis, read our post ‘5 Steps To Develop A Diagnosis In Physical Therapy‘.)
Mistake #2: Confusing a Single Treatment as the Solution
This mistake is almost as common as the lack of a working diagnosis (Mistake #1).
When someone uses the same treatment on every person, there is an assumption about what is the problem. The most common combination is a patient being told they have muscle tightness and scar tissue everywhere. The solution is vigorous massage or dry needling or active release or myofascial stretching or some variation of muscle treatment. This could be the right answer for the occasional individual with just a muscle injury, but often it becomes an endless treatment plan.
A treatment is not a solution.
A treatment is not rehab, its just a treatment.
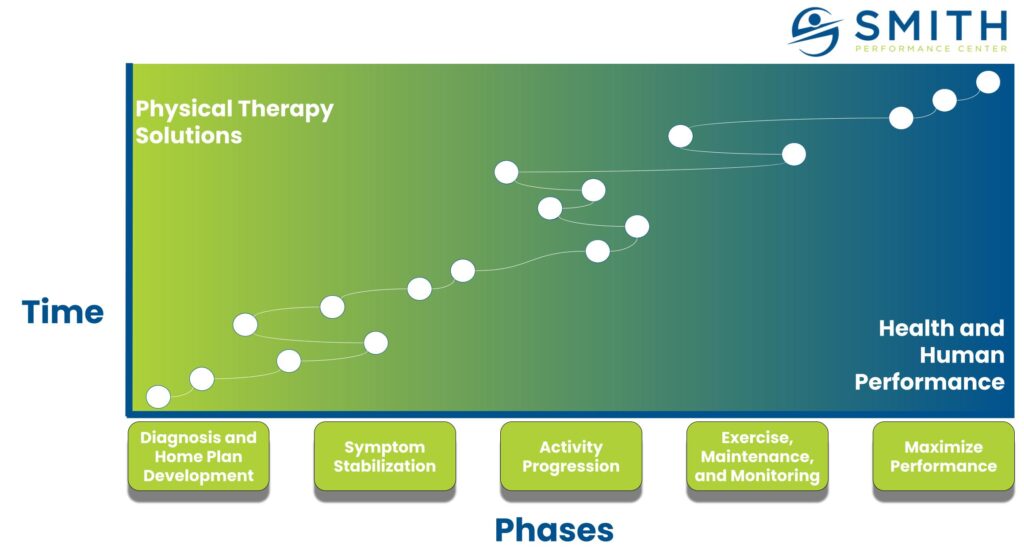
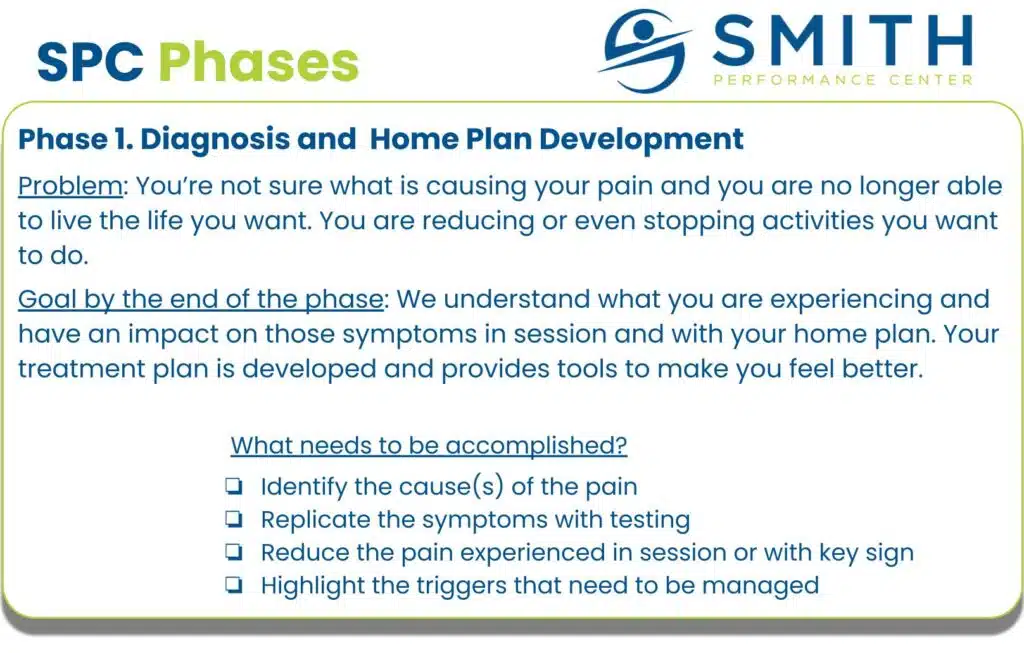
Solution #2: Get a Plan of Care with a Supported Process
Manual treatments are a great way to start getting people better, but for successful rehab, there needs to be clear metrics that you as a patient can evaluate the progression of rehab.
We do this with our SPC Phases. At each phase, there is a different problem that needs to be addressed. During Diagnosis and Home Plan Development, we want to confirm the pain generator. We are not out of this phase until we know the cause of the pain and have been able to improve it (see the example below).
This combined with a working diagnosis and differential list (Solution #1), a clear home plan (Solution #4), and retesting after providing treatments (Solution #3) leads the provider to use whatever combination of manual treatments, exercise, activity, and planning that makes you better.
A single treatment is not the answer – a process is.
Mistake #3: Lack of Retesting the Exam
I find it insane, but some patients who walk in have never actually had testing to recreate the problem.
Patients who have had an exam often never have it done again. When I first started practicing, I remember seeing patients who were impressed by a physician that could diagnose the problem within seconds. The physician had seen this numerous times. It sounds cool until it became clear the diagnosis was not correct. Now it sounds lazy. (Learn more about the diagnostic process HERE)
There are so many ways to mess up a diagnosis and the lack of an exam and retesting it for success means you are flying blind with rehab.
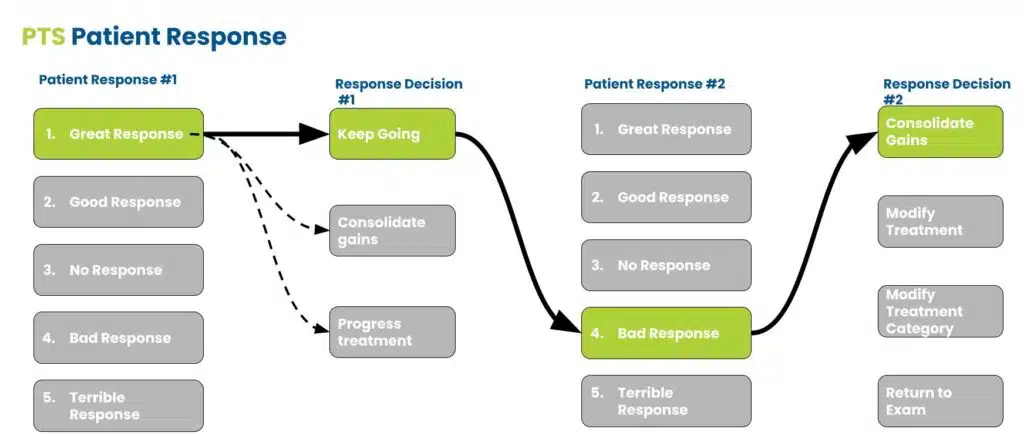
Solution #3: Multiple Exams in the Same Session
We do the exam numerous times.
Our team searches for things we call key signs that most effectively recreate the main symptom that brought you in. We retest it over and over again to measure the success of our treatment within the session. This allows us to confirm our working diagnosis (Solution #1) and create an effective treatment strategy that you can do at home (Solution #4).
Mistake #4: Stopping the Activity
Imagine you are a runner.
You go to the doctor and you tell them you have knee pain with running. What do you think you will be diagnosed with and what do you think the treatment will be? My guess is you will be told you have Runners Knee and the solution is to stop running. And you had to pay for that!
So you stop running and like magic, the pain gets better.
You start running again a month or two later and the pain returns. Our term for stopping the activity – Fake Improvement. There are few situations where stopping the activity is helpful.
Stopping the activity without a clear action plan is the biggest mistake in orthopedics because there is no guarantee it will resolve.
Solution #4: Clear Home Plan Including Trigger Management Plan
A more effective solution is to understand all of the things contributing to the pain.
If a runner comes in with knee pain, this can be due to the patellar tendon, meniscus lesions, or irritation of the knee joint just to name a few. Runner’s knee is a garbage catch-all term saying that you run and you have knee pain (Mistake #1). The pain could be due to a lack of warm-up or an inhibition problem that occurs with running that can be solved with banded side steps every couple of miles.
The running itself is not the problem, rather a change in your neuromuscular system is.
When you stop running, you never get to test the solutions and you get stuck in an endless loop of starting and stopping. A home plan takes into account what works in a session as demonstrated by retesting (Solution #3) and gets you the tools to do it at home. A trigger management plan helps you figure out what other things may be contributing, like sitting down right after a run may increase your knee pain. To manage the trigger, you do not sit down within 30 minutes of running.
This means that activity that you were going to stop can actually become therapeutic!
Mistake #5: Confusing Rehab with Long Term Programming (also known as the endless home exercise list)
While some people may disagree with us, the idea that the physical therapy exercise list is something you need to do for a lifetime is not sustainable for 99% of humans on planet earth. It is time-consuming, lacks a real plan, and uses exercises focused on rehabilitation.
Solution #5: Use a Supported Exercise Program
No matter what you do, after you have an injury there is an elevated risk it will come back.
All the information out there on preventing injury is typically a person peddling the next injury-prevention cure. Once you are done with rehab, you need to get back to the activity that maximizes your enjoyment and your health. We go after the problem of recurrence, and chronicity, and support active lifestyles in different ways. If we are worried about the pain returning, we develop an action plan that is used once the problem seems to return.
You apply the plan as soon as needed.
The point is that an endless exercise list does not prevent the problem from coming back. The focus needs to be on lifelong activity and catching problems right when they start. You want to gain resilience, which you can do with numerous tools, and get the benefits of an active lifestyle.
What if you just go with whoever your insurance covers?
When you decide on where to go and what to do with your rehab, this list will help.
It does not matter if it is at a busy insurance-based clinic, the chiro down the street, or a famous orthopedist that treats the best athletes in the world. Your case and your presentation are unique because you are unique. If you don’t consider the mistakes and solutions, you become a passive patient with no control over your rehab plan.This is a big mistake and can lead to more visits, more pain, and reduced quality of life. Even in busy clinics or intimidating office visits, make sure you get the care you want.
This list will help you ask questions and evaluate the plan you get.