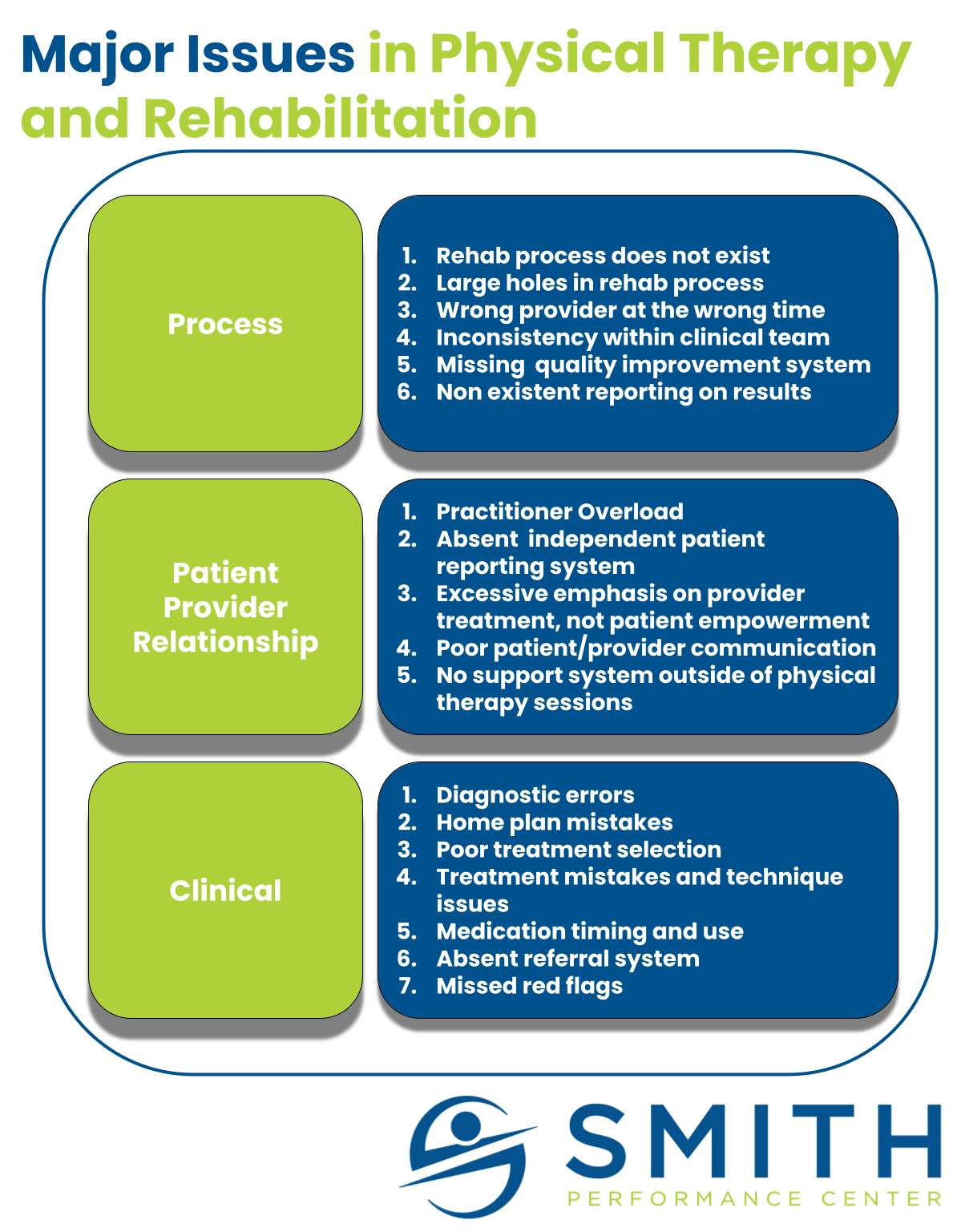
A structured rehab process that ultimately targets a full return to activity is missing in healthcare.
Patients struggling with pain are treated as if they are all the same. We believe there are common, big problems to address, but there is a high degree of uncertainty with every patient presentation. Even when a patient has the same diagnosis they can have different triggers, different contributing factors, different behaviors, and drastically different needs in the rehab process. This is true when patients have the same surgery by the same surgeon.
Let me use an example with a straightforward rehab plan; post-total knee replacement.
The Painful Total Knee Replacement
Peter Pain had a total knee replacement.
He has always been active and handles pain well but this replacement has been horrible. First, he fell behind on medication post-surgery because he hated the way the drugs made his stomach feel. The second day was horrible and he never managed to get in front of the pain train. At home, he slept with his knee slightly flexed for the first two weeks because of pain. Physical therapy did not start at home because his wife was sick and he did not want anyone at the house. When he arrived at physical therapy, the physical therapist noted a severe range of motion limitation. When the therapist handed Peter off to his assistant, the pain exploded even with light activity.
Peter is in trouble.
Peter dealt with the agonizing pain of getting the knee bent over a couple of months, the motion gains seemed to disappear after each session, and the exercise hurt.
Fast forward two months and the pain is now manageable if he does nothing – limited walking, minimal movement, and no exercise. He never gained his range of motion. Walking for more than a couple of minutes increases pain dramatically, so he doesn’t walk even though that was the main reason he decided on surgery. He stopped physical therapy and continues his home exercises but they typically make his knee feel worse.
Peter believes surgery was a terrible decision.
Peter has a complex presentation despite having a common surgery.
The Painless Total Knee Replacement
Phyllis Flexible had a total knee replacement on the same day as Peter Pain.
Phyllis has been told she is hypermobile, meaning she has more elastin in her connective tissue. When she walks the day after the surgery, her pain medication is working and the pain is minimal, maybe even a little less than prior to the surgery. Her quad fires easily and before she gets discharged to go home she is able to do a straight leg raise for almost 25 repetitions. She regains full knee range of motion within the first 2 weeks without
Phyllis independently stopped her medication on the third-day post surgery because her pain was not a problem.
By the time she showed up for physical therapy, she was able to walk without pain. The physical therapist quickly evaluated her knee and Phyllis spent 45 minutes with an assistant doing exercises. The extra time spent on exercise makes Phyllis feel even better. She is now getting into shape in a way that she never could when her knee hurt.
Phyllis believes surgery was the best decision of her life.
Phyllis has a simple presentation despite having the same surgery.
The Tale of Two Knees
Peter and Phyllis had the same surgical procedure, but their care at physical therapy should be drastically different.
There is a good chance Peter will have permanent issues with his knee unless the physical therapist makes a lot of great choices, monitors his response, doses activity, unloads appropriately, and Peter follows through on the plan as prescribed. Phyllis probably could have skipped rehab and been fine; generic rehab is more than sufficient. Peter, in contrast, is screwed. He will fail in most rehab situations because generic rehab will ignore his out-of-control pain cycle and poor trigger management. Overuse of assistants and a heavy emphasis on using exercises that hurt will make the pain cycle worse.
Despite similar problems leading them to surgery, they now have different problems, different challenges, and different needs.
Peter does not understand what is causing his pain and does not have a helpful home plan. We call this phase 1 – Diagnosis and Home Plan Development.
Phyllis is ready to progress her activity and needs support to keep her knee healthy for the long term. This occurs in phase 3 – Activity Progression.
Addressing the Right Problem at the Right Time
When Peter walked in the door of our clinic, he did not want to be there.
He joked that he thought PT stood for ‘physical terrorist.’ It’s hard to disagree considering what he has been through with the generic rehab that Peter received. The therapist forced painful flexion for months. All his current PT exercises increased his pain. Loading the knee for his “sit to stands” and the prescribed walking regimen caused a dull throbbing that grew in intensity until he couldn’t keep moving. Outside of the ice and e-stim at the end of the session, he felt worse after each session.
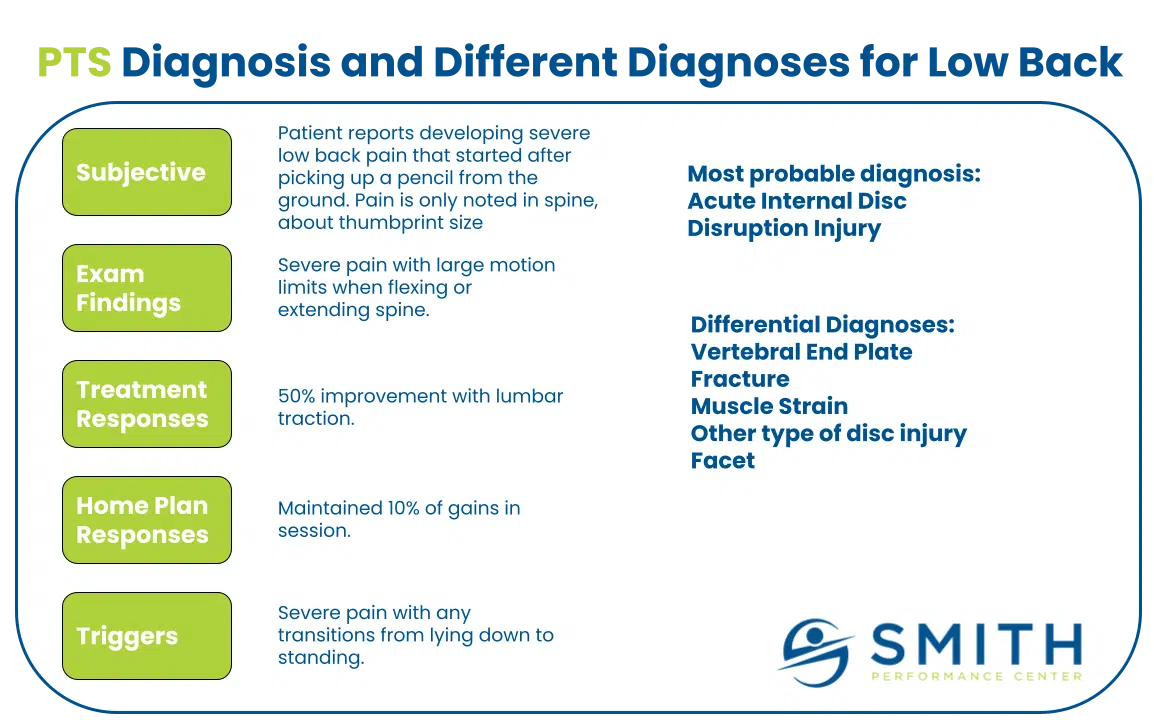
For our team, Peter is solidly in our Diagnosis and Home Development Phase.
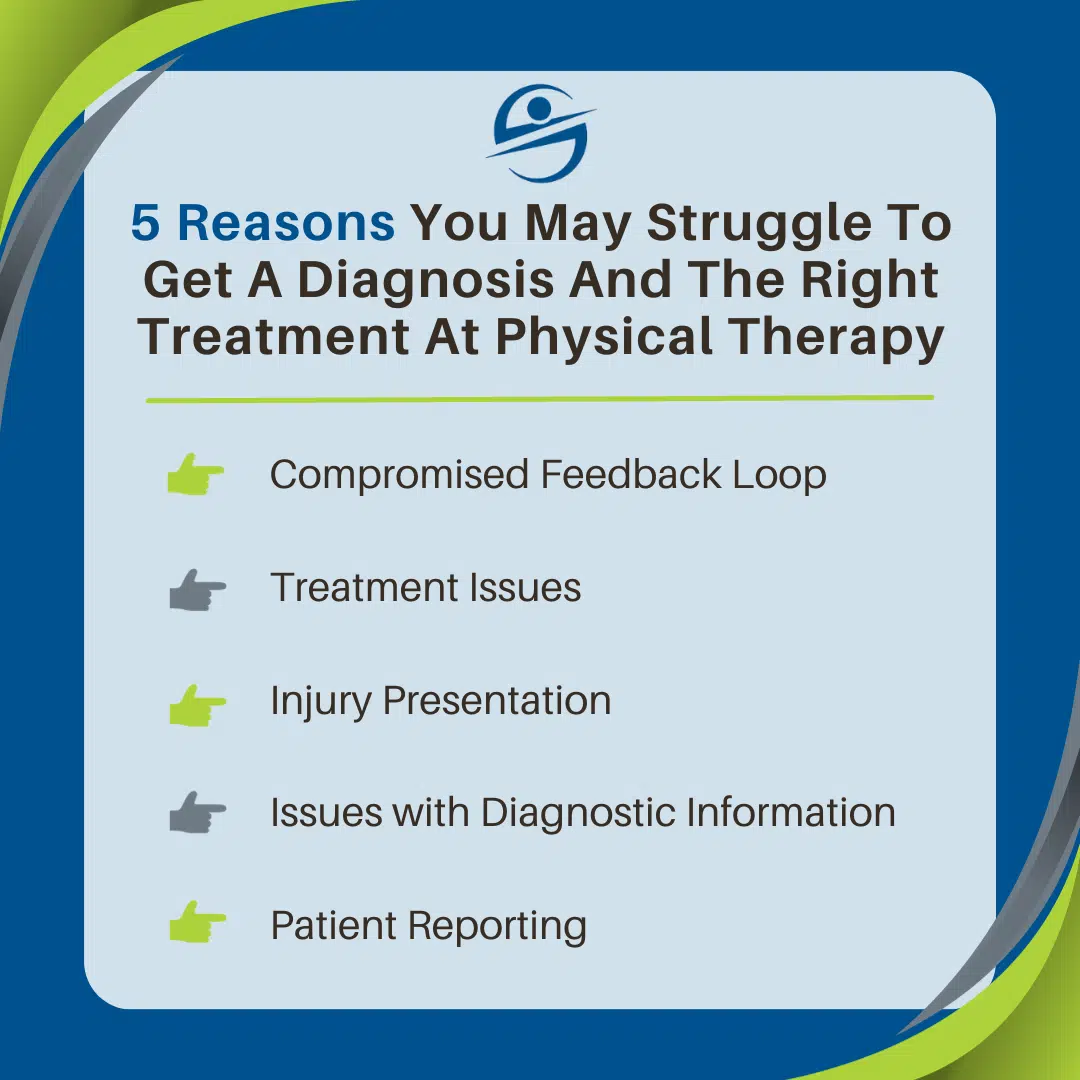
Physical therapy must determine everything that is causing his pain.
In this situation, the natural assumption is the total knee surgery but this was not Peter’s issue. He had seen the surgeon and there was another x-ray. They ruled out infection. He decided against going under anesthesia and having the surgeon bend his knee to break up any adhesion.
So, the entire first visit is a deep dive into everything that could cause his pain.
We examined his knee. He had pain with passive knee flexion, knee extension, resisted knee flexion, and knee resisted knee extension. The surgical scar was exquisitely painful. The knee appeared swollen and radiated heat. The muscles of the quad and hamstring were painful to the touch with numerous trigger points that sent shocks of pain into the knee. The exam also found pain with a passive range of motion at his hip and an inability to produce force with hip abduction. Peter could not perform a single leg calf raise. Not only could he not perform it, but the attempt caused severe pain when his knee moved into extension.
There were numerous pain generators present.
We dove into treatment, using the treatment hierarchy.
Our key signs to retest for positive responses were passive knee extension and standing pain. We performed massage on the quad. There was no change. We performed light traction to the knee. This reduced pain with standing but only by 10%. By this time, the session was over. From the exam, it is clear that he is triggering his pain with every step he takes, any time he stands up, when he sits in his recliner with his leg straight, and when he sleeps at night. (Read more on how we use patient responses to direct our treatment and home plan.)
The target for the home plan will be getting a pain reduction with knee extension.
We built a plan that started to address all of his daily triggers. The current PT exercise list was eliminated because every exercise was painful. We gave him a cane and put a heel lift in the shoe to prevent full knee extension. This reduced walking pain by 90%. His sleep position was adjusted so the knee did not hurt with sleep. This meant he had a significant knee bend, which is typically discouraged because it causes a contracture to form (meaning the knee loses the motion), but if sleep remained painful, he would only continue to lose more motion, develop more pain, and get further into his current problem.
Peter returned one week later.
He had a 50% reduction in pain with walking. Knee passive motion remained painful. Soft tissue massage trigger point release to the quad was more effective, reducing standing pain by 80%. This confirmed his quad was a significant pain contributor. We also understood that the uncontrolled trigger of knee extension, occurring during standing, walking, sitting reclined, and his sleep position must be controlled until passive knee extension is pain-free.
The same home plan is used and added in self-massage to the quad.
After a lengthy discussion, Peter promised to keep using the cane no matter what for the next week.
His pain is 90% better the next week and his diagnosis is updated to include myogenic pain from the quad.
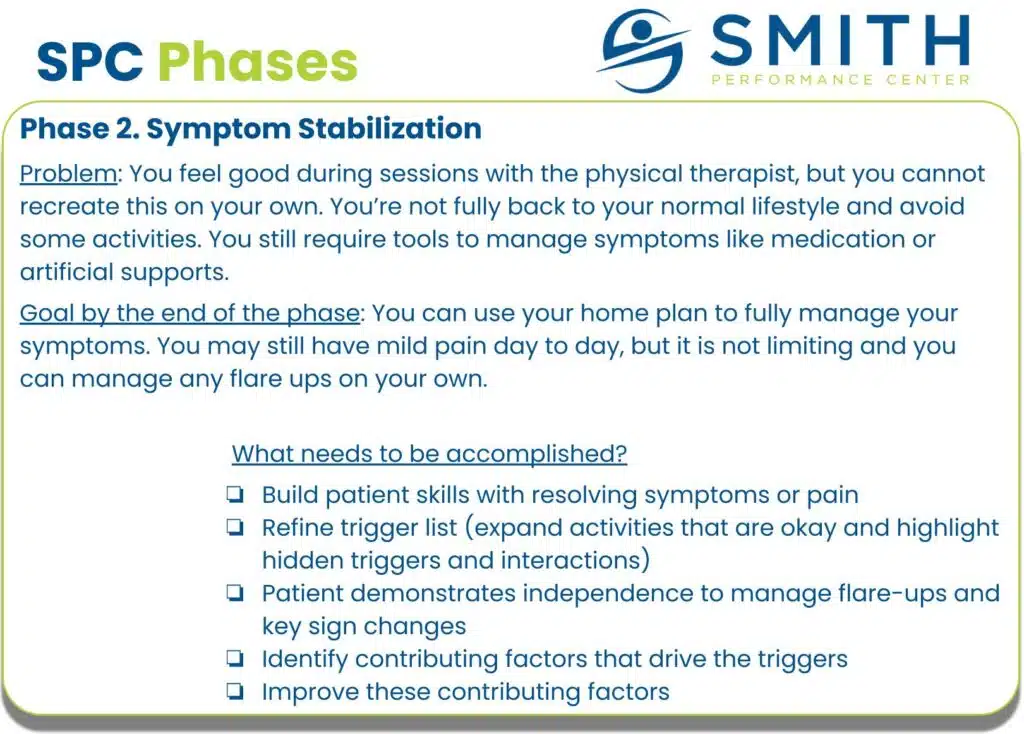
We have accomplished the goal for phase 1 and we decide to move to phase 2 where Peter is more effective on his own.
Remember, Peter is terrible at managing his own symptoms and this phase will take much longer.
His natural inclination is to ignore pain, but that strategy is not going to work. When the treatment progresses to address his impairments list (knee range of motion, walking gait, muscle strength at glutes, quad, and calf, motor control, sensorimotor system, pain), most of the gains will be lost if Peter does not manage his pain. This will take training and a couple of setbacks, but he will develop the needed skills to deal with any pain increase in his knee.
So we started to work on Peter’s ability to make himself feel better, his current, and his current, biggest problem.
Understand and develop a plan around your current problem
One in five people who report being unhappy with their total knee one year after the replacement (Bourne 2010, Madhi 2020). But in this situation, the surgery was not the problem. The initial clinical process that treated Peter with a one-size-fits-all treatment plan caused Peter’s problem to get worse. Not everyone is Phyllis. While we did not address her situation in this article, the focus on Phyllis should be supporting her move toward an active lifestyle.
The process matters.