Why should I go to Physical Therapy Solutions at Smith Performance Center for my knee injury instead of another clinic?
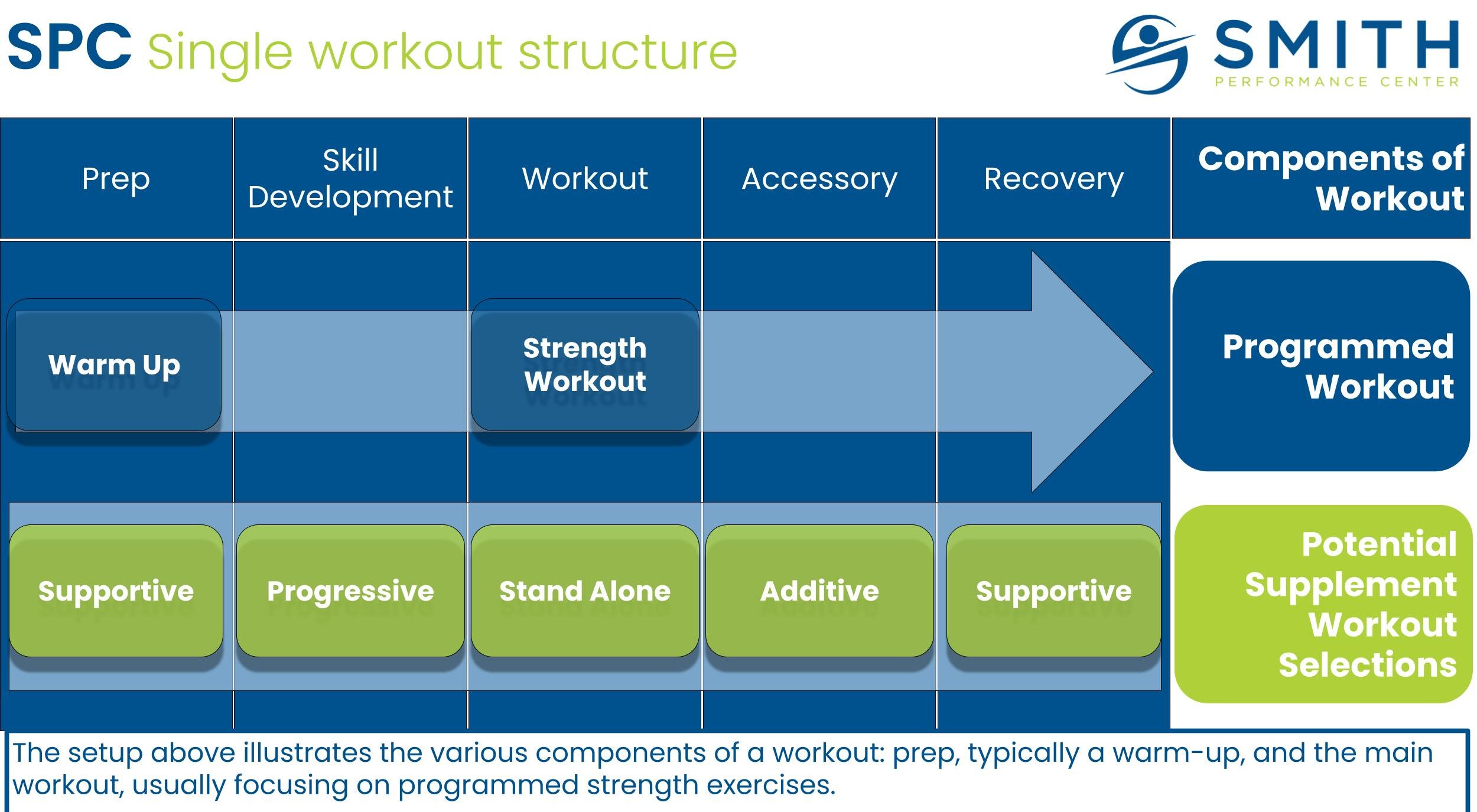
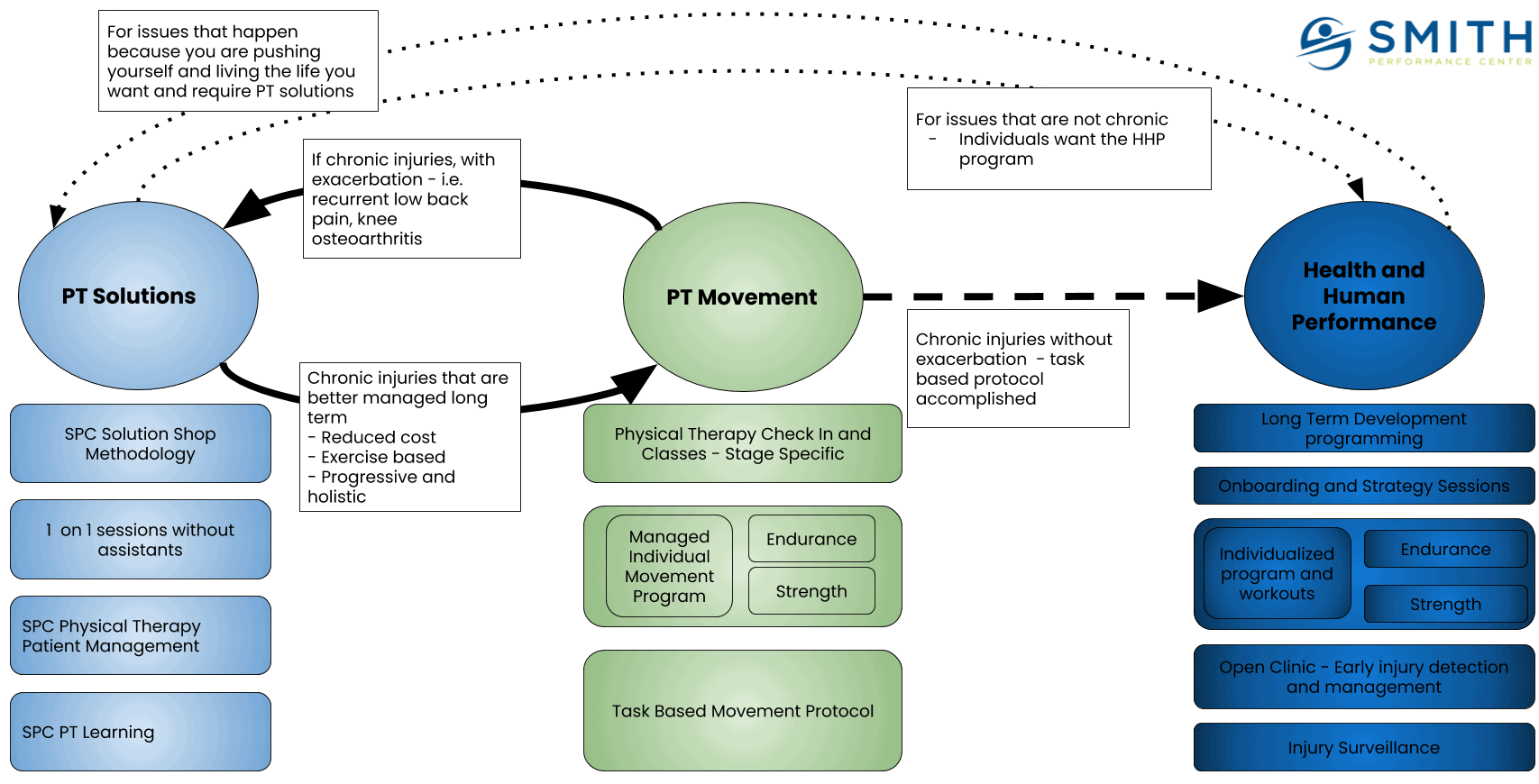
Physical therapy at Smith Performance Center is not a cookie-cutter, one size fits all type of operation. Depending on what problem you have, the ‘right’ service might be different. Our process, called the SPC Difference, uses physical therapy in 3 distinct services:
PT Solutions – One on One Physical Therapy Sessions using SPC Methodology
PT Movement – Group Physical Therapy Sessions using Task Based Protocol for recurrent, chronic, or post surgical injuries
Health and Human Performance – Long term strength and movement programming your own coach including injury surveillance, early injury detection, and treatment integration
 Physical Therapy Solutions
Physical Therapy Solutions
The knee has numerous structures and dysfunctions that can contribute to the pain a person experiences.
If there is a meniscus degeneration, is that causing the pain? Maybe…but there are studies on people without knee pain that have meniscal degeneration. There are even studies of people showing the same injury on both knees with only one knee that is painful.
If imaging shows knee joint space narrowing? Maybe…but there are studies in people with severe knee osteoarthritis without knee pain that show ‘bone on bone’.
What if the clinical exam is negative but there is constant pain with standing? Or walking? Or steps?
The pain could be due to the meniscus, the bone, the cartilage, the patellar tendon, or the ligaments. We need to avoid quick answers that we cannot verify. We need to think and test our hypothesis and see that our treatments lead to less pain. We need to test and track your response. We need to stick with it until you feel better.
PT solutions can be thought of as physical therapy consulting: we figure out your problem as quickly as possible, develop a workable solution, and get back in control.
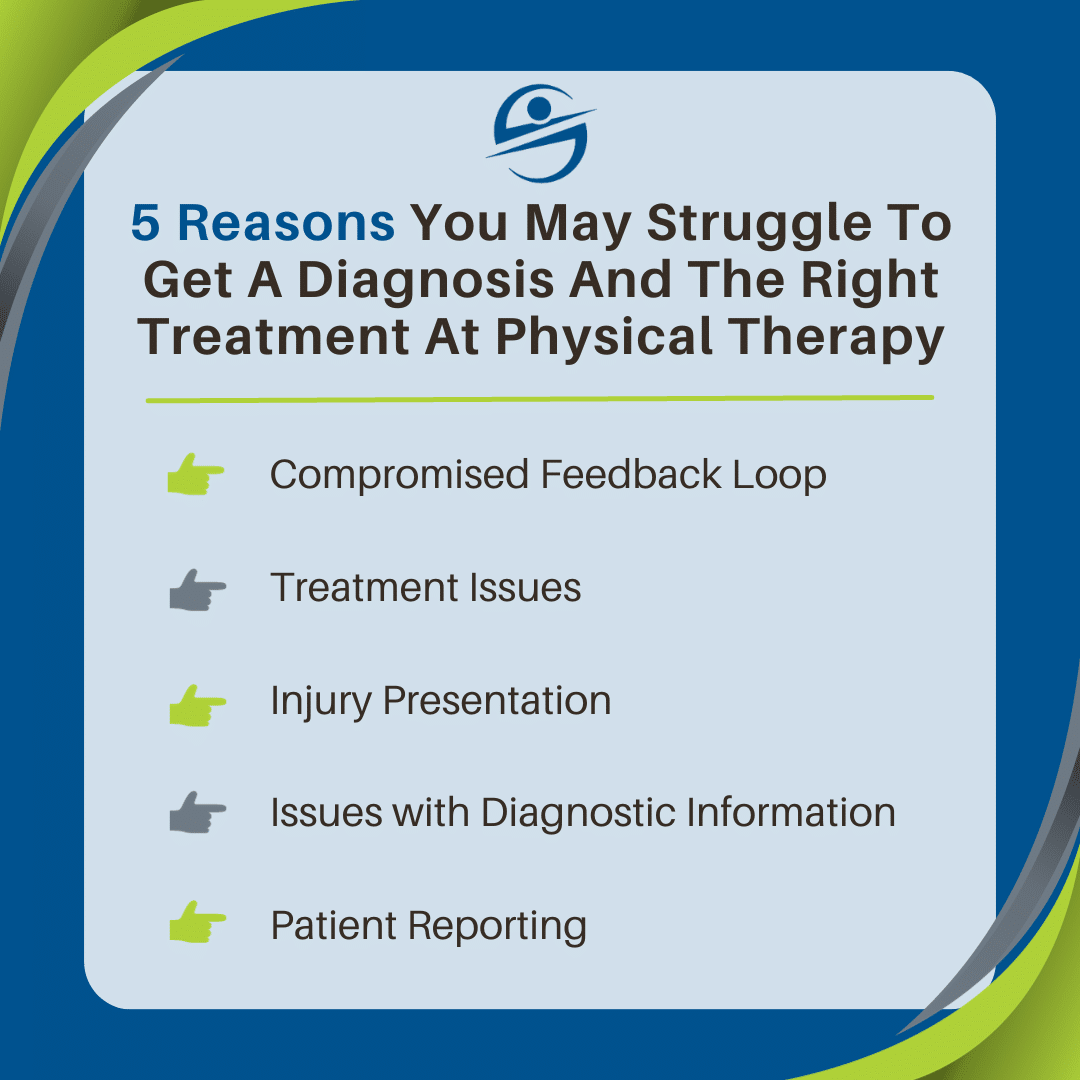
When you understand this thought process, then you understand why we do the following:
One-on-one sessions without assistants: if there is not a clear strategy, why would we pass you off to an assistant?
Hour-long sessions: We do not want to be rushed and make cognitive mistakes because of it.
Team Collaboration: We use our collective experience to review the majority of cases, especially in difficult cases that are not getting better.
In-depth home plans: We want you to own the problem and understand what is happening. The success hinges on the 167 hours you are not with us.
Trigger Management: We want a clear understanding of what is causing your symptoms.
Minimize Activity Reduction: We know many providers tell you to stop doing painful activities. We call this ‘fake improvement’ because nothing is really being fixed. We want to maintain as much of your normal activity as possible because injury and pain are the number one factors in becoming sedentary. If you can get better while maintaining your normal life, then we know we have the right solution.
Manual Therapy: We use hands-on techniques to relieve pain and improve tissue quality. This can give us a window of time to implement the home plan.
3-level prognosis: We provide a range of visits using best-case, worst-case, and expected scenarios so you understand the cost and your role in making the best case happen when possible.
Limited treatment sessions: We do not use your pain as a tool to extract as many visits as possible. We try to have one visit per week as this helps us test our hypotheses and get better results. If you are doing well and we have a treatment scheduled, then we cancel it or move it to the next week. We will never over-treat when you do not need it.
Example of Manual Therapy
Knee Traction
When is Smith Performance Center not the best place for you?
We are not for everyone and there are situations where we encourage individuals to use their insurance and use us as a resource.
Our physical therapy team views itself as a problem-solving machine. For knee injuries, we specialize in injuries that seem to keep coming back or do not resolve when you go to other places. We like hard, complex problems without clear solutions along with easy, straightforward problems that we can quickly solve.
However, this requires a commitment to working on the problem with us. The best results occur with clients that follow the home plan and provide feedback on what is working and what is not working. If you have difficulty following a plan, then that will be one of the biggest barriers to getting better. Other physical therapy clinics will schedule multiple sessions per week, and in the situation where you cannot do the home plan, this type of setup may be better suited for you.
We do not use modalities or bikes. We are not trying to get as many billable units as possible. When our session starts, the focus is on the highest-value activities. We will spend the session trying to understand the problem, testing our hypothesis, and building out the home plan you will be following. If you go to physical therapy for passive modalities beyond hands-on manual therapy, then Smith Performance Center will not likely be the right place for you.
Common knee problems we treat
Knee pain with running downhill
Downhill running is a large eccentric load to the quad. Every foot strike can lead to loads many times that of the body. We often forget this because of how easily we do it. There can be numerous reasons for the pain:
Joint irritation: there is swelling in the knee joint for a bad landing or some other trauma. The swelling leads to the quad not firing well which leads to more joint irritation.
Excessive knee extension at landing: The strategy when running downhill may be shifting the load from the quad absorbing forces eccentrically to the knee joint. This can happen from a previous pain state or from poor technique.
Poor quad strength: the quad may not be strong enough to handle the eccentric load. . In these cases, the best problem may be PT Movement as thousands of monitored reps will be needed.
Quad inhibition: the quad may be getting shut off during the run. The pain happens after two or three downhills in the same run.
Quad Overactivation: The quad is a strong and the most critical muscle in downhill running. Occasionally, the quad will start to fire too much. It will feel like the muscles get tighter and tighter during repeated downhill sessions. In later stages of this problem, you will feel that the quad over activates even in flats. Other indicators are feeling that the quad muscle is always tight, the hamstrings cramp easily, your back starts to hurt when you try to stretch your quad, quad cramping, and generalized quad achiness.
Calf weakness: The calf is responsible for controlling tibial advancement in midstance to terminal stance. If this is weak, then the gait cycle changes and will require the runner to shift the pattern to compensate. This is a common pattern after low back injury that included undiagnosed compromise of the S1 nerve root. We will see one calf is much smaller than the other. We will test calf raises and see that one cannot perform even quarter of the reps as the other, unaffected leg.
Gluteal inhibition: the glute is important for controlling lower extremity absorption. The gluteals can be inhibited by a variety of issues including: low back pain, hip pain, knee pain, ankle pain, ankle sprain, and likely other causes.
Gluteal weakness: Sometimes if the gluteal inhibition has been going on long enough, then there is actual weakness that develops. This is not as common as you may think. If this is the case, then once the pain is managed, we encourage you to join the Health and Human Performance Program as true weakness needs anywhere from 6 to 12 months to fully recover.
This is not an exhaustive list but each of these problems requires a different approach. It is not as simple as glute exercises or quad stretching.
Knee pain, motion loss, and the recommendation for surgery
There are indications for surgery however many times there are options that can be used to prevent surgery. When surgery is needed, then we can make sure you are ready for it.
A common problem we see is knee pain with large motion loss and imaging that shows nasty osteoarthritis. In these situations, we find the most basic steps in rehab have been skipped and previous physical therapy, chiropractic, or specialist treatment has not addressed the root problems.
Here is an example:
There are three situations in which a quad will not function properly – pain, motion loss, and effusion. If you try to do quad-strengthening exercises, nothing will stick. You have to diligently get rid of at least one of these problems. At Smith Performance, we normally start with pain.
You may be thinking, where the heck would you start? In these situations, there is often a patellar tendinopathy and quad myofascial dysfunction along with knee-activated osteoarthritis. We will start by making the quad feel better, unloading the knee joint, and retraining the quad light activation exercises. During this pain-reducing stage, the most critical factor is to get you, the patient, onboard and committed to unloading until the pain is gone. Once this happens, we can address the other two issues of effusion and motion loss. After we get those two issues under control, we rebuild the quad while constantly monitoring for setbacks.
When I review the notes of patients that fail at other clinics, often there is nothing in the notes about the knee joint effusion (swelling). The treatment was normally exercise based with an assistant that actually made the pain worse because the knee could not handle the extra load. This is disappointing because in many cases this situation responds well to rehabilitation and physical therapy, just not mindless, poorly constructed workouts.
Knee pain that keeps coming back
Who has not had knee pain at least once? In recurrent knee pain, the same problem seems to keep occurring. This is common in people who like specific activities that make the knee hurt – hiking, running, walking, sitting, standing, stairs, lifting, yoga, biking, soccer, basketball, football, baseball, and work. That may seem like most activities a person can do.
The point is that once the injury happens, you are likely to get it again, especially with activities that caused it in the first place. The goal of treatment is to understand what is the culprit and build a plan for it.
The goal should not be to take time off. This does not solve the problem.
Knee pain and your doctor says there is nothing wrong
If you have pain, there is something wrong. This happens regularly because imaging and the physical exam are not sensitive enough to catch every problem. When we do not recreate the problem in the first session, often we make go do the activity until we can capture the problem in an exam. If the exam remains negative, you will go back to all of your normal activity and have our physical therapy session right after the activity that causes the pain.
Knee pain stopping you from living the life you want
We do not want to go through every possible knee injury that could bring you in to see us. The biggest reason to come to Smith Performance Center for our one-on-one physical therapy is to figure out the problem, build a solution, and return to the life you want to live.
How do we get you back to a life without knee pain?
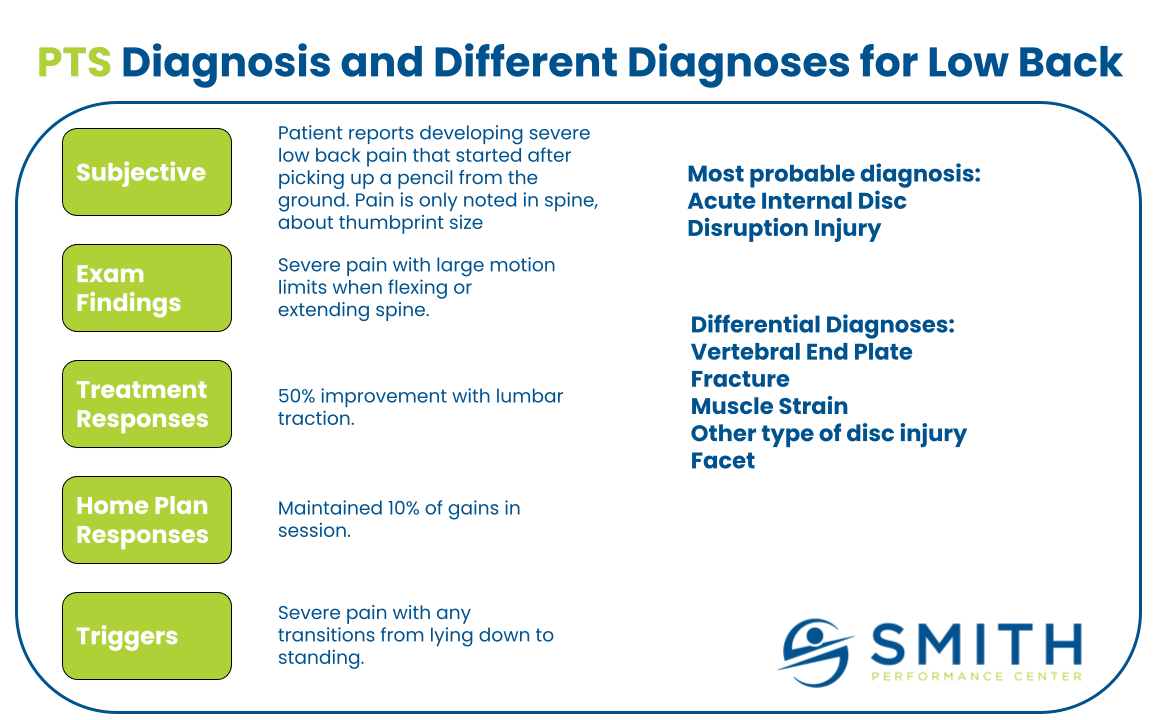
Step 1: Understand the problem from your perspective
Step 2: Build a diagnosis from your medical history, subjective, objective (physical exam)
You can learn about this process in the article, Diagnosis in Physical Therapy.
Step 3: Test the diagnosis using your subjective and objective key sign
Step 4. Retest in the same session until an effective treatment is found
Step 5: Develop a home plan including recovery positions, exercises and activities, and trigger management strategies
It is easy to forget about triggers, but they can be the difference between success and failure.
Trigger Management in Physical Therapy
Step 6: Create 3 Level Prognosis
We believe it is critical to understand the uncertainty in medicine and physical therapy. We can use this uncertainty to build a better plan using the 3 Level Prognosis.
Step 7: At follow-up sessions, refine the diagnosis and the home plan
This may include braces, taping, training aids, or specific exercises.
Step 8: At discharge, integrate the home plan into the normal daily routine
Do you want to schedule an appointment?
Physical Therapy Session

 Physical Therapy Solutions
Physical Therapy Solutions