Updated by Craig Smith February 22, 2025
Understanding Knee Pain: Why Won’t It Go Away?
Knee pain is a common and persistent problem that affects daily life. Whether you’re avoiding stairs, switching from running to biking, or waiting for a knee replacement, chronic knee pain can disrupt your routine.
And it is more complicated than we often admit or see online.
At Smith Performance Center, we believe that effective knee pain treatment requires more than just exercises or quick fixes—it needs a structured plan. This is where our SPC Phases come into play. Our phase-based system ensures that each step of rehab is intentional, guiding patients from pain relief to long-term performance.
This article explores why knee pain occurs, how physical therapy should address it, and what steps you can take to regain control over your movement.
Why Is Knee Pain So Common?
The knee may seem like a simple hinge joint, but it’s far more complex. It absorbs and transfers forces between the hip and foot, cycles through multiple gait phases while walking, and relies on precise coordination between bones, ligaments, muscles, and cartilage.
When pain begins, you may unconsciously adjust your movement to protect the knee—sometimes at the expense of long-term joint health along with compensatory changes due to strength or sensory changes. The changes in walking patterns can indicate underlying pathology, or changes in muscle strength.

Key Structures That Can Cause Knee Pain:
- Meniscus – Cartilage that cushions the femur and tibia, vulnerable to tears under excessive force. Learn more about meniscus degeneration and treatment approaches in our detailed article: Knee Pain, Meniscus Degeneration, and Clinical Experience.
- Extensor Mechanism – Includes the quadriceps, patellar tendon, and supporting connective tissues essential for knee stability.
- Joint Surfaces – The tibiofemoral joint experiences wear and tear, contributing to osteoarthritis.
- Ligaments and Tendons – Provide structural support and can become strained or inflamed.
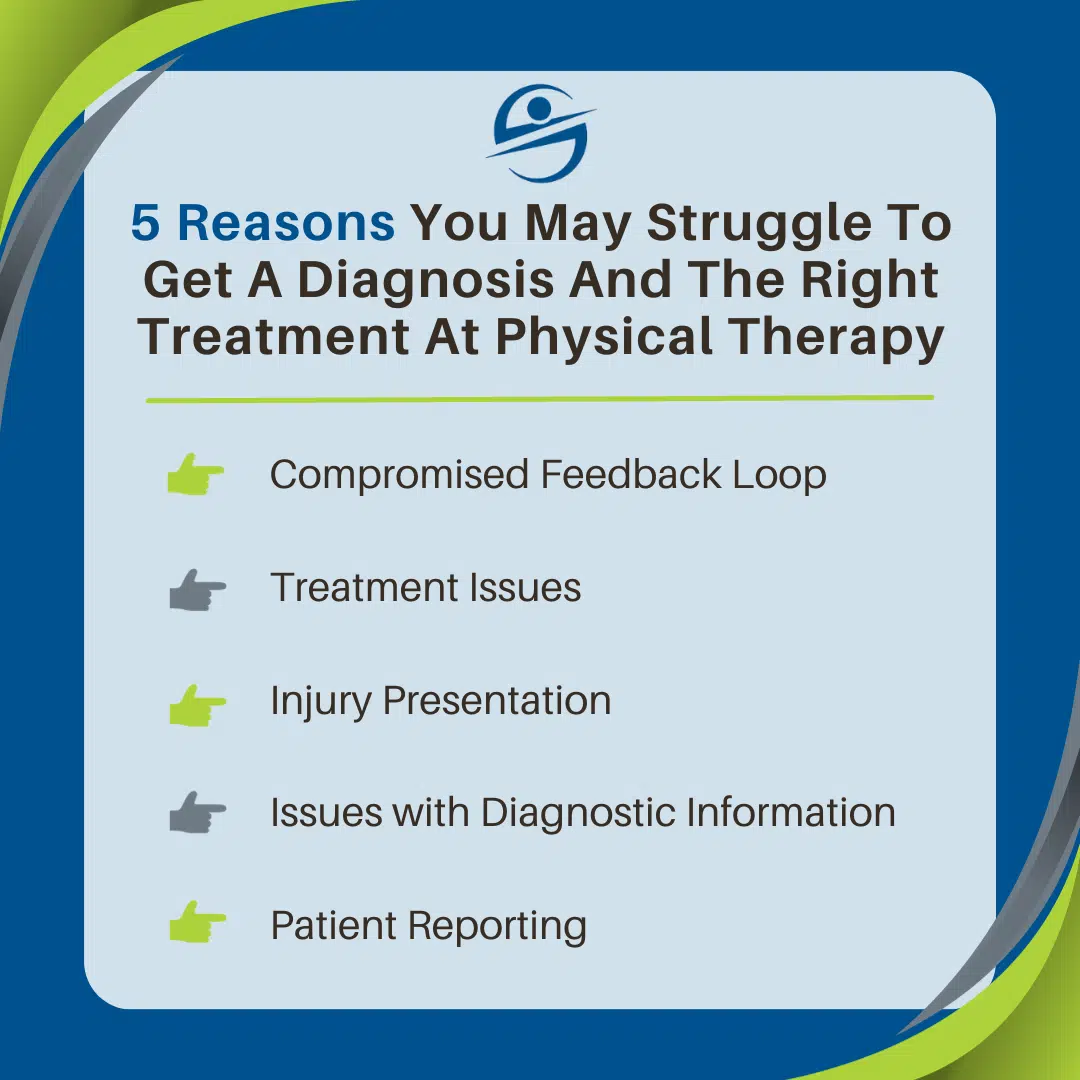
With so many potential pain generators, the first step in rehabilitation is getting the right diagnosis. This is where Phase 1 of the SPC system begins: Diagnosis and Home Plan Development.
The Physical Therapy Process: A Phase-Based Approach
Effective knee pain treatment requires a systematic and progressive plan. At Smith Performance Center, we use a five-phase system to ensure you progress safely and efficiently. Here’s how it works:
Phase 1: Diagnosis and Home Plan Development
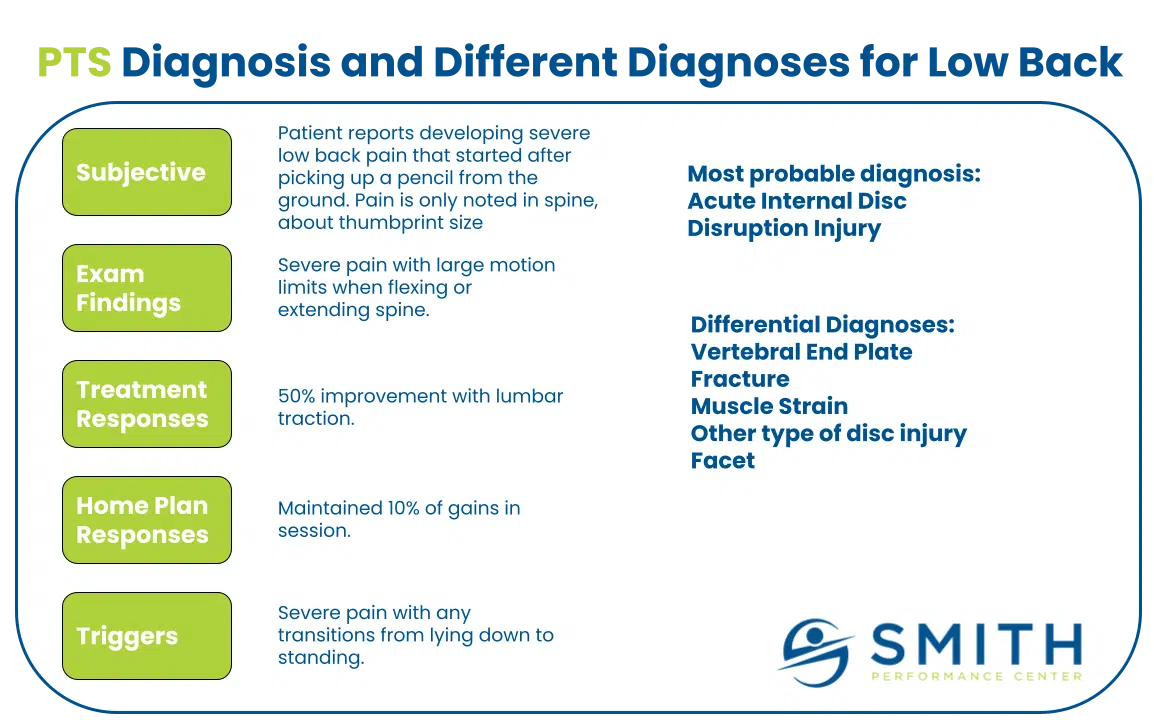
Your treatment must start with a clear understanding of the problem. A working diagnosis means updating our hypothesis as we gather more information. For example, while knee osteoarthritis may appear to be the main issue, pain could be driven by an irritated patellar tendon. To confirm the diagnosis, we focus on making symptoms better during the session. If symptoms improve, it supports our diagnosis; if not, we reassess and refine our approach. Without identifying the correct pain generator, treatment will not be effective.
Phase 1 is about confirming the diagnosis by making symptoms better in-session. If we apply a specific intervention—like knee traction, a SERF strap, or movement modification—and it reduces pain within a session, we gain confidence in our approach. If symptoms don’t improve, we reevaluate and refine our strategy. Most non-surgical knee injuries should show measurable improvement in the first session.
Phase 2: Symptom Stabilization
Phase 2 focuses on empowering the client to take full control of their symptoms. By this stage, they should consistently make their symptoms better without direct therapist intervention. Our goal is to ensure that they can recognize early signs of flare-ups and address them independently with proven strategies, minimizing setbacks and maintaining progress. By this stage, clients should have the ability to manage their symptoms independently, applying the strategies learned in therapy to consistently improve their condition without direct therapist intervention. Our goal is to ensure that they can handle flare-ups independently, recognizing and addressing issues as they arise.
Phase 3: Activity Progression
A successful treatment plan extends beyond physical therapy sessions. This phase is about building tissue capacity to tolerate greater activity demands. A well-structured home plan should:
- Address daily triggers (e.g., This includes hidden and obvious triggers such as modifying movement patterns, using a cane for unloading, or managing joint swelling). Learn more about overcoming invisible triggers that may be stalling your rehab progress in our detailed article: 7 Tools to Overcome Invisible Triggers.
- Avoid exercises that aggravate symptoms (e.g., endless squats and step-ups often do more harm than good), and be mindful of activity creep—where you gradually increase activity levels without realizing it, leading to unexpected flare-ups.
- Focus on effectiveness, not just effort (e.g., symptom relief and movement restoration should take priority over generic strengthening). We call this the rehab standard, and it’s important to keep the focus on tissue capacity, not just exercise capacity. Tissue capacity refers to the ability of muscles, tendons, and joints to tolerate load and stress without breakdown or pain, while exercise capacity is simply how much activity someone can complete. Prioritizing tissue capacity ensures the body is truly prepared for increasing demands, reducing the risk of reinjury. Learn more about progressing workouts safely after an injury in our detailed article: The 5 Most Useful Tools for Progressing Your Workouts After an Injury..
Phase 4: Exercise, Maintenance, and Monitoring
As symptoms improve, the focus shifts to sustaining progress through targeted strength and mobility work. Regular exercise becomes a key component, as research shows that even conditions like osteoarthritis respond well to movement rather than avoidance. Studies have shown that structured exercise programs can reduce pain, improve function, and slow disease progression. While it may seem counterintuitive, avoiding activity often worsens symptoms, leading to greater stiffness, pain, and functional decline. Exercise helps strengthen the muscles supporting the knee, improves joint lubrication through synovial fluid production, and regulates inflammation, making it a critical part of long-term symptom management. This phase prevents recurrence and builds resilience, ensuring you don’t fall back into the cycle of pain.
Phase 5: Maximize Performance
For those looking to return to high-level activity or sport, performance training bridges the gap between rehab and full function. This is where we focus on specific objective goals determined by the individual. This includes force absorption drills, sport-specific conditioning, and loading strategies to prepare the knee for long-term durability.
Diagnosing Common Knee Pathologies
At Smith Performance Center, we perform a basic exam, evaluate movements, and categorize knee pain based on movement restrictions, pain patterns and treatment responses.
Here are common scenarios:
- Pain when straightening the knee → Anterior horn meniscus compression which responds well to Meniscal tibial mobs, terminal knee extension exercises, and tools like a heel lift to reduce knee extension during the gait cycle.
- Pain when bending the knee → Joint restriction, osteoarthritis, or meniscus tear. Traction helps alongside normalizing the force absorption chain of the quad, glutes, and pretibials.
- Sudden loss of knee motion with swelling → Traumatic synovitis (joint irritation). Reduce the overload of the joint, long hold traction, and quad activation. Managing swelling is critical, as persistent swelling inhibits quad activation, leading to ongoing dysfunction.
- Long-term swelling and stiffness → Chronic osteoarthritis. There are typically 4 issues here, loss of knee extension, loss of knee flexion, chronic swelling combined with quad atrophy. All four of these factors must be addressed together for effective pain management.
- Loss of quad strength or persistent tightness → Extensor mechanism injury or patellar tendinopathy. To optimize recovery, we need to enhance tendon and muscle tissue quality, improve force absorption mechanics, and proactively manage overloading and hidden triggers.
Each of these patterns requires a unique treatment approach. A blanket treatment strategy won’t work—precision matters.
Your Next Steps: What to Ask Your Physical Therapist
If you are dealing with knee pain, you should demand clear answers from your provider. Ask these key questions:
- What is my diagnosis? (Understanding the pain generator is critical.)
- **What is my main problem? **
- What is the functional cause? (What movement or behavior contributes to my pain?)
- What is my home plan? (A structured plan should go beyond a generic exercise list.)
- What are my daily triggers? (Avoid vague recommendations like “stop running” without context. See Phase 4: Exercise, Maintenance, and Monitoring for more on how regular exercise, even for osteoarthritis, is essential for recovery rather than avoidance.)
At Smith Performance Center, our goal is to help you take control of your knee pain and return to the activities you love. If you’re not local, we hope this guide empowers you to make informed decisions when working with other physical therapists.
Need Help?
If you’re looking for personalized treatment for knee pain, our team at Smith Performance Center is here to help.
Schedule a physical therapy evaluation or Movement Assessment at Smith Performance Center today!