An invisible trigger is a problem that can stop you from fully healing.
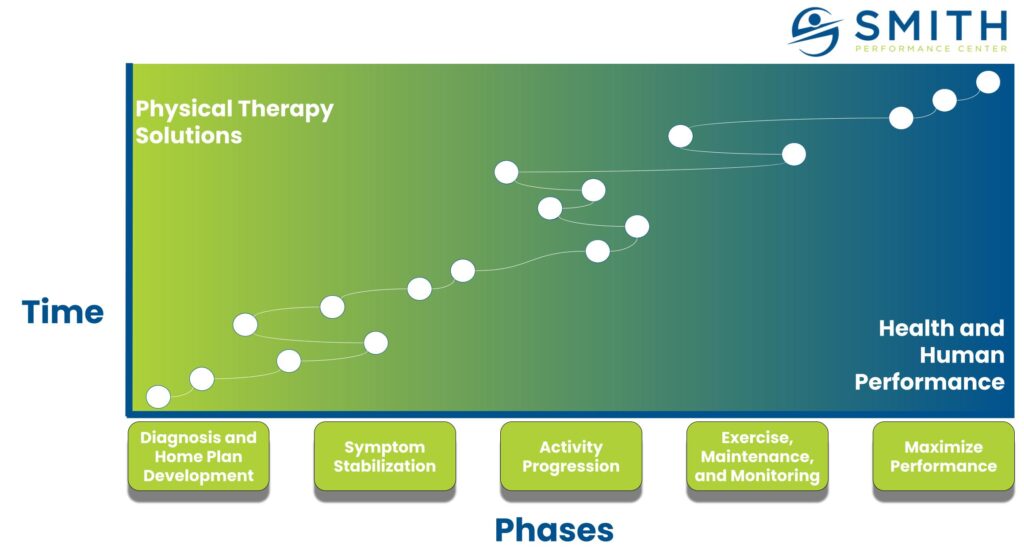
An invisible trigger is an action or activity that does not seem to be causing your injury to worsen but is actually causing your injury to remain and not heal properly. During the course of treatment, our team comes across this problem frequently when a patient will seem to stop progressing in their rehab plan. This problem presents most often during the symptom stabilization and the activity progression phases. The physical therapist will see an improvement in symptoms during a session, but then progress is lost when the patient tries to manage the symptoms on their own. During activity progression, there is often an interaction between the activity being progressed and normal daily activities.
 Do you have this problem?
Do you have this problem?
If you say yes to the following, an invisible trigger is not being addressed.
- Pain keeps returning when you try to do more activity.
- There are random increases in pain without a clear cause.
- Your feedback loop on pain is not immediate, but delayed.
- You have plateaued in your rehab progress.
- You have great results in session or even great results for a few weeks but then your improvement seems to disappear.
If this describes you, there are tools to get you back in control.
The 7 Tools to overcome invisible triggers
There are 7 tools to use when dealing with invisible triggers.
- Control variables – Limit new variables in your rehab plan
- Develop a key sign – Use key signs linked to your symptoms that are more sensitive than your overall symptoms
- Focus on key sign improvement – Use the home plan to improve your key signs while monitoring for what activities cause the key sign to worsen
- Understand your feedback loop – Document when your primary symptoms occur and what you did between one flare-up and the next
- Monitor exercise with controlled progression – Use a monitored exercise program during activity progression
- Activity interaction elimination – Eliminate common interactions between activity and sustained positions
- Use artificial stabilization – Use tools to help manage your triggers
1) Control variables
Managing an invisible trigger requires good information.
The more variables you have to consider, the more difficult the trigger will be to manage and overcome. Consider the following scenario with a triathlete dealing with low back pain. Cycling volume was assumed to be the cause of their returning pain. However, their hidden triggers happened to be track work for running and time spent sitting. Cycling did not have an impact on their pain. However, this client added all of these things at the same time and the assumption of cycling as the cause of symptoms was never challenged until we conducted a discovery session testing cycling as an issue.
We had the client ride their bike for one hour without symptoms.
Now by having a baseline we went back to all of their other activities and tested them for being hidden triggers. Running caused pain but the symptoms were delayed by about one hour. Sitting was symptomatic within 2 hours. We added running on days without biking to test for increases in pain and limited sitting to 30 minutes at a time. These variables were controlled and not changed for one week to make sure the patient experienced no symptoms.
After a week, we could decide what would be the next variable to progress.
2) Develop a key sign
Key signs are the most important tool for invisible trigger management.
The key sign is an activity or movement that you can use to test for irritation of your problem before you actually feel symptoms. For example, you may have back pain that only shows up in the morning. During the day, your symptoms will not help in determining what activities cause pain in the morning. Instead, we use forward flexion and extension of the low back. If these feel stiff, tight, or painful, after sitting for 60 minutes, we know this contributes to your morning low back pain.
Being able to catch a flare-up or activity that causes your symptoms means you now focus on the key sign, not the symptoms that brought you to rehab
3) Focus on key sign improvement
The key sign is the feedback tool, not your pain when there is an invisible trigger present.
To use the example above, If the key sign remains pain-free, the pain in the morning will not increase. This is an assumption and your physical therapist will test this with you. Once a key sign is tied to later symptoms, we focus on making sure the key sign does not get worse. There are two prominent methods to make the key sign feel better: use your home plan to improve the key sign and avoid activities that make the key sign worse. For the back pain example above, we may use lumbar traction to make the forward flexion and extension feel pain-free – this is making the key sign better. We also avoid sitting for more than 60 minutes because this makes the key sign worse.
Rehab efforts focus on the key sign.
4) Understand your symptom feedback loop
An absent or delayed feedback loop can devastate the rehab process.
If you have no idea if an activity causes your pain, it is difficult to know if your current activity needs to be modified, supported, or eliminated. We try to get around this by doing an exam and eliciting pain. This helps to get a diagnosis. However, our therapists and coaches frequently encounter clients reporting a random increase in symptoms but it is not really random.
The first answer to this problem is to get key signs to monitor as proxies. The second answer is to monitor and document when your symptoms occur. Look at what preceded one pain symptom and the next. Write everything down that occurred in the previous 24 hours.
5) Monitor exercise with controlled progressions
Monitored exercise with controlled progressions allows for previous client experiences to be applied to your problem.
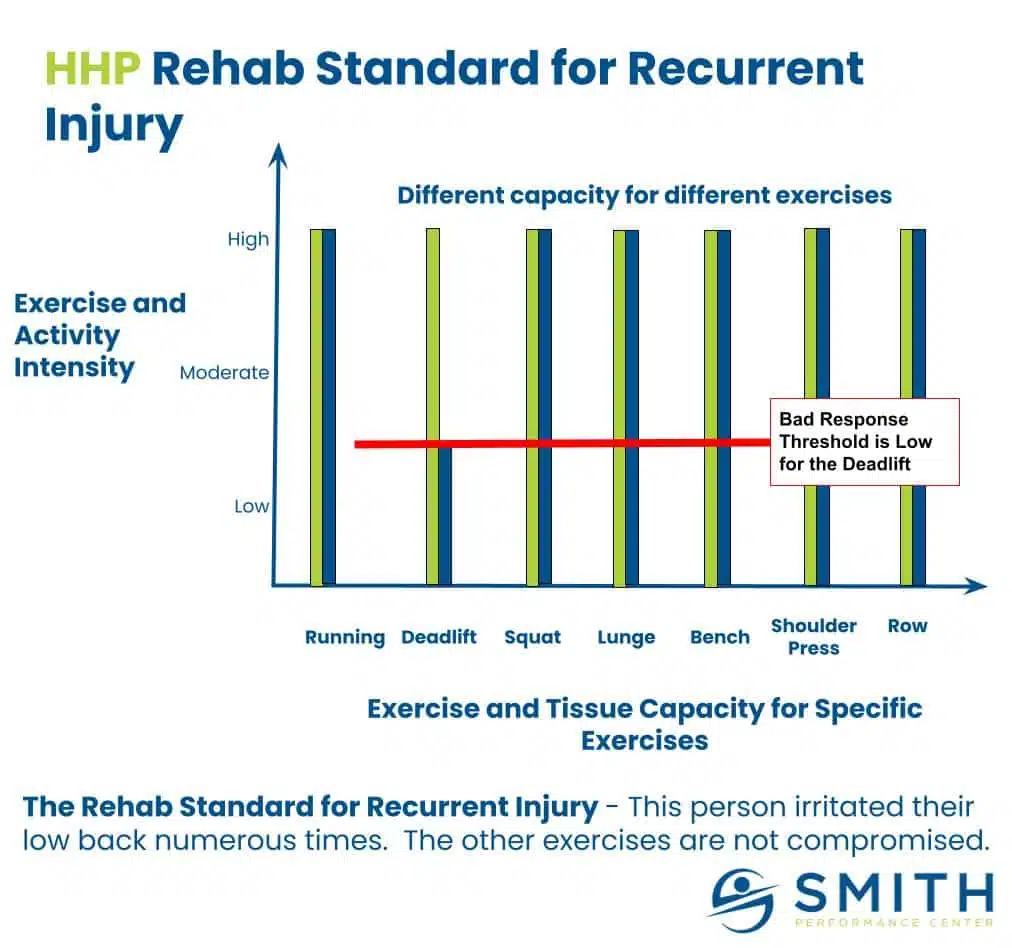
A common complaint occurs when a patient surpasses their tissue capacity due to their ability to exercise at a high level. Our team calls this the rehab standard meaning you need to limit progression to what the tissue can handle.
Having a standard, monitored, exercise progression prevents invisible triggers from stopping your activity. You can determine which exercise families contribute to your pain. In the example above, we should look at all lower extremity pull exercises as possible triggers to symptoms.
6) Activity interaction elimination
Activity interactions mean an action followed by another action causes the symptoms, while either action happening on its own is not a problem.
Activity interactions are common. We see them occur with a dynamic repetitive activity followed by prolonged positioning. Think walking followed by sitting or biking followed by standing. The dynamic repetitive activity irritates the tissue and the prolonged positioning exacerbates the irritation.
Search through your day for any of these types of interactions. If you cannot completely avoid it, then break up the time during the repetitive activity and the prolonged position.
7) Use artificial stabilization
Artificial stabilization uses taping, bracing, or external support to reduce or resolve symptoms.
Artificial stabilization is a concept from our physical therapy team. There is a negative view on bracing but for invisible triggers, it can prevent normally provocative activities that are stalling your rehab progress from becoming a big issue. We use this strategy in a multitude of ways:
- Modified low dye for pain on the bottom of the foot
- Lumbar brace for pain with sitting or transitional activities
- SERF strap for poor glute use during running
- Cervical collar for pain when sleeping
- Post-tib brace for pain during loading response of gait
- Heel lift to unload the Achilles tendon during terminal stance
These are just a few examples. For invisible triggers, it can allow us to test for a suspected cause of pain. If you think sleep is causing your low back pain, you can use the brace when sleeping at night. If we think walking is causing your knee pain due to incomplete knee extension, we can put a heel lift in the shoe.
These are treatment tools and not crutches that need to be used for the rest of your life. Often once the invisible trigger is resolved, these tools can be retired.
Your turn to use the tools
Our team developed these tools after working successfully with thousands of people. If you get stuck during rehab, it’s not hopeless. To get back on track, think about where you are in the rehab process and test these tools.
If you need help or would like to talk further about your issue, let our team know!