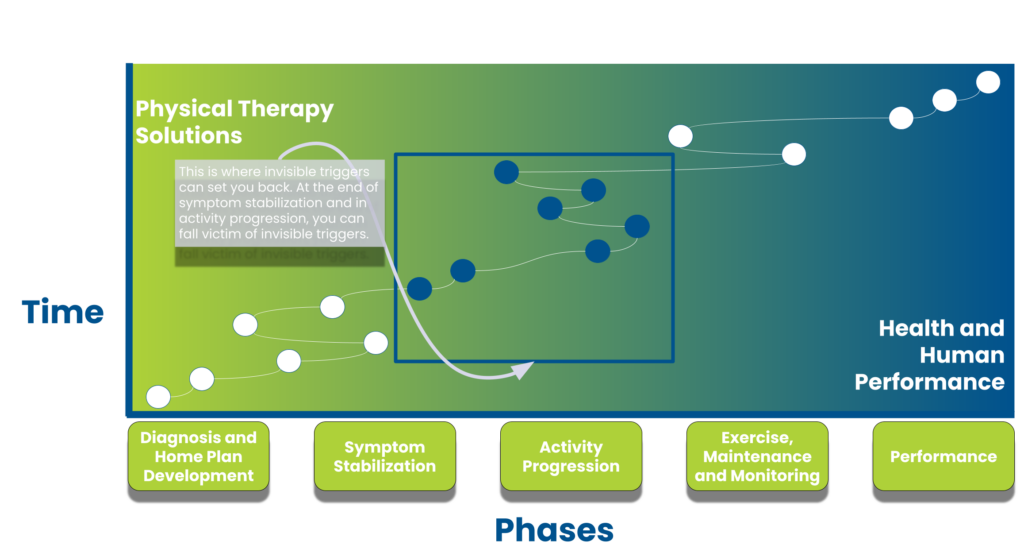
You keep getting close to feeling good but then fall back into an injury because of a common, but often unrecognized issue – invisible triggers.
An invisible trigger is an action or activity that does not seem to be causing your injury to worsen but is actually causing your injury to remain and not heal. If you slammed your finger into a door, you would know the door caused your pain. Continuing to slam your finger in the door will cause the finger pain to remain.
In contrast, an invisible trigger is not as clear as slamming your finger in a door.
Patients have an easier time eliminating obvious triggers. This does not happen with invisible triggers. An example would be low back pain triggered by an interaction between two activities: running followed by a bout of sitting. When we investigate running by itself, there is no problem. We repeat the same procedure for sitting and there is no problem. However, running followed by sitting led to low back pain within 30 minutes.
This is an invisible trigger with components of a delayed feedback loop (there was a 30-minute delay) and activity interaction (running and sitting caused pain; neither caused pain by themselves).
The key is that invisible triggers are not obvious and rehab progress can stall when you miss invisible triggers.
5 components of invisible triggers
There are 5 components of frequently seen invisible triggers that stall rehab progress:
- Low Barrier to Repetitive Action – the invisible trigger is an activity that you can do for a significant time or significant repetitions without an immediate pain increase but as the time/repetitions continue, symptoms can develop.
- Delayed Feedback Loop – The pain is not immediate after an activity and symptoms can appear random or unrelated to the triggering activity.
- Activity Interaction – A single activity is pain-free but can be painful based on what activities precede it.
- Trained Brain Trap – You have trained yourself to do an activity that blocks the recognition of symptoms.
- The Familiarity Trap – The activity is something you have always done without pain in the past.
Low barrier to repetitive action
Repetitive activities are the concern here, especially those that are pain-free for the first reps.
We think about walking, biking, or swimming. Anything that you can keep doing and perform thousands of times without immediate pain. The problem is microtrauma to the body or an inhibition response in the muscle. This is very common in knee, shoulder, and low back injuries. Going from 1,000 to 10,000 steps is easy but to your knee that is a 10-fold increase in load. You may feel great at 1,000 steps but a jump to 10,000 steps will ultimately blow up the pain.
The invisible trigger is the volume of the repetitive activity, not the activity itself.
The key is to monitor activities that can be easily and repetitively performed.
Delayed feedback loop
The delayed feedback loop is one of the most challenging aspects to manage during the rehab process.
The delayed feedback loop hinders rehab progression by hiding the cause of the pain. The invisible trigger inciting event is separated from the patient noticing symptoms by time, ranging from an hour to 24 hours. A common class of pathologies with delayed feedback loops is spine injuries. Patients report a great day but then wake up with severe pain. They focus on the pain all day and stick to the home plan and the pain slowly resolves. The next morning the pain is good again and they resume a normal amount of activity. As the day progresses they feel even better. The next morning, all of the pain is back again.
We often hear our patients blaming the bed (which it can be in some cases, but not when we see this type of yo-yo in response).
The activity the day before is the inciting event, but the pain does not present for almost 12 hours.
The key is to notice how your pain and feedback loop present.
Activity interaction
Your daily actions do not happen in a vacuum.
There is constant interaction between the activities you do in a day. When you have an injury, a common invisible trigger is activity interaction. As we mentioned above, the two activities when performed at different times cause no issues, but when one is done and immediately followed by the other, pain results. Often it’s an activity followed by a sustained position. Think running followed by sitting. Biking followed by standing at a desk. Swimming followed by a 30-minute car ride.
A trigger journal can be critical and we often use this to uncover the cause of headaches.
The trained brain trap
The brain trained to focus may miss signs that your symptoms are increasing.
This issue is common in knowledge workers who sit or stand in a sustained position for a long time and get lost in their work. Engagement in the activity means the symptoms are not initially noticed. We also notice this in individuals who disassociate in some ways from their bodies. They will have a hard time noticing symptoms and will be prime candidates for invisible triggers.
The trained brain trap means you have to put in scheduled stops to check for symptoms that increase as you will not notice otherwise.
The familiarity trap
Familiarity can also make some patients actually notice subtle differences and pick up problems sooner, but this is not everyone!
The more familiar you are with an activity, the easier it is to perform. Your ability to do the activity increases the likelihood you can do it and not recognize symptoms. This accounts for some of the problems seen in the components above. You can run on autopilot, missing that your ankle is starting to feel tight. The hundreds of hours running before may make the new symptoms harder to note.
Most invisible triggers may present with one or more components
As you can see from above, these components have crossover in their presentations.
The key to understanding an invisible trigger is to monitor your response to activity closely. If you have a delayed feedback loop, you need to write down what activity you are doing. If you have pain after an activity that was pain-free, look at the preceding activity. If you can get lost in an activity, use a tool to bring awareness back to your symptoms in time intervals.
Without this information, your rehab progress can stall.