Returning to Activity, Physical Therapy, and Neuromuscular Fatigue
Neuromuscular fatigue has been implicated as a significant problem for individuals returning to sport following an anterior cruciate ligament (ACL) injury and reconstruction. Due to the high rate of re-injury in those that have had an ACL reconstruction, one hypothesis is that neuromuscular fatigue will negatively impact strength performance, postural stability (single leg balance), and biomechanics during jumping and landing. It blows my mind that a female athlete with an ACL tear is 16 times more likely than a healthy female athlete to tear an ACL again.
The interplay between a previous injury, the resulting changes to the input to the brain, modified motor planning, and re-injury is an interesting development in research. Today I wanted to dive a little more into fatigue, its impact on biomechanics, and how physical therapy and strength training can start to augment the problem.
There are direct implications for any knee injury, especially to the joints and ligaments. If you have knee osteoarthritis, recurring knee pain, or an old knee surgery, this information is important to know. It may keep your injury from coming back.
Fatigue?
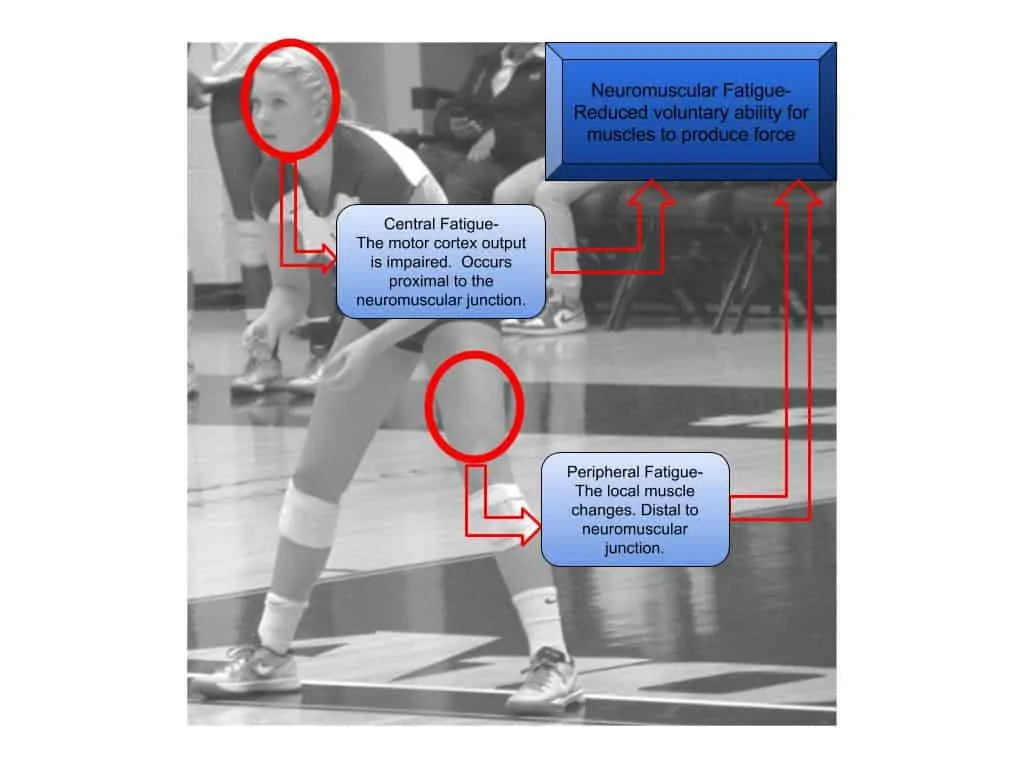
Neuromuscular fatigue is a decrease in the ability of an athlete to produce voluntary force in a muscle or group of muscles (McLean), which is a combination of central and peripheral fatigue. Peripheral fatigue is related to muscle damage and metabolic factors distal to the connection between the motor neuron and muscle fiber. Central fatigue can occur anywhere prior to the connection between the muscle and motor neuron (Figure 1). On the surface, quantifying or even getting a clear view of central fatigue seems impossible to examine in detail with any moving or jumping test. When I was reading over all the information on fatigue, I kept imagining when I ran a 400-meter race in track (just a horrible experience). The first two hundred meters felt fine but by the final curve, my ability to run and pick my legs up was basically gone. This fatigue was due to the metabolic byproducts produced from all-out effort along with bumping against a central governor.
Testing
A repeated finding for individuals with ACL reconstruction is a consistent deficit of strength in the quads, hamstring, and glutes. This has been measured in a variety of ways. It can be an isometric, strength exercise, or functional pattern. At Smith Performance Center, we use a hand dynamometer, step-down test, and strength norms with lifts.
Single-leg balance is also a critical component that can capture brain changes that are not expected. We commented on this before that balance can become impaired if visual dominance develops. Our preferred method of single-leg balance testing is the Y balance test however this requires the eyes to be open and will not quantify visual dominance unless stroboscopic glasses are used. This has been an interesting tool that I will dive into later. If you want more information, I wrote an article for lower extremity review here.
There are also numerous landing tasks that can be performed. A consistent finding has been that an athlete who tears their ACL demonstrates risky movements during jumping, landing, cutting, and pivoting. These movements appear to remain even after physical therapy and the rehabilitation process. This is a large problem since most ACL injuries are occurring during these types of movements and the rehab process is not successfully improving the movements. Our research has been focused on the tuck jump assessment and hop testing, but there are multiple ways to examine the strategies that an individual is using.
Overlaying all of these findings is the fact that performance deteriorates with fatigue. Unfortunately, neuromuscular fatigue appears to hit those with a peripheral joint injury more (Ie. ACL injury).
Let’s dive into the research.
The Research
Thomas, A. C., Lepley, L. K., Wojtys, E. M., McLean, S. G. & Palmieri-Smith, R. M. Effects of neuromuscular fatigue on quadriceps strength and activation and knee biomechanics in individuals post-anterior cruciate ligament reconstruction and healthy adults. J Orthop Sports Phys Ther 45, 1042–1050 (2015).
The authors tested quad strength, central activation ratio, and knee biomechanics before and after the fatigue protocol in a group of individuals with ACLR and a control group (no ACL injury). The central activation ratio was an interesting concept. The max voluntary isometric contraction of the quad (variable one) was performed by the subject then it was followed by an electrical stimulus to get the highest contraction possible (variable two). To get the central activation ratio, they used the following formula:
central activation ratio=maximal voluntary isometric contraction with electrical stimulus
The ACLR group was significantly weaker than the control group and landed with a stiff-legged landing pattern. No difference was seen in the central activation ratio between groups, however, a significant change did occur within the group after the fatigue protocol. The fatigue protocol did not exaggerate this difference between the groups.
Frank, B. S., Gilsdorf, C. M., Goerger, B. M., Prentice, W. E. & Padua, D. A. Neuromuscular fatigue alters postural control and sagittal plane hip biomechanics in active females with anterior cruciate ligament reconstruction. Sports Health 6, 301–308 (2014).
The authors did not run a true experiment as there was no control group. Their subjects were individuals who had a recent ACL reconstruction. The authors looked at the change in biomechanics and single-leg balance pre and post-fatigue protocol. Similar to the other papers, a reduction in hip flexion was seen. Single-leg balance was also impaired.
Mclean, S. G. & Samorezov, J. E. Fatigue-Induced ACL Injury Risk Stems from a Degradation in Central Control: Medicine & Science in Sports & Exercise 41, 1662–1673 (2009).
This was an interesting and thought-provoking article. The authors wanted to investigate the impact of neuromuscular fatigue along with a cognitively demanding task. The authors looked at the change in the landing biomechanics of each leg following a fatigue protocol.
Here was the setup:
Pre-fatigue: The subjects were asked to jump based on the light signal.
1. Light 1 meant jump from both feet, land on the left, and immediately cut laterally to the right.
2. Light 2 meant jump from both feet, land on the right, and immediately cut laterally to the left.
3. Light 3 meant jump vertically from both feet and landing on both feet
To test the cognitive load, for some of the jumps the light would switch on approx. 5 seconds before the subject jumped. This allowed for planning. To add the unanticipated component, the light would not go off until the subject jumped. So while in the air, the subject would get this light signal and have to immediately make the jump upon landing.
Fatigue Protocol
1. 3 single leg squats followed by random jump protocol until 3 squats in a row could not be completed without assistance
2. The jumping biomechanics was monitored throughout this entire fatigue protocol with the randomized jumping tasks.
Knee flexion at initial contact and peak stance was reduced (more stiff-legged landing) along with increases in hip internal rotation and knee abduction angles following the fatigue protocol. Unanticipated landings with fatigue protocol resulted in even greater hip internal rotation and knee abduction angles.
Physical Therapy Takeaways
Clinically, I have not seen the application of fatigue protocols consistently. A true fatigue protocol will take time. Take the following studies for example:
1. Repeated sets of 8 squats to 90 degrees of knee flexion followed by 3 dynamic jumps until the participant cannot perform the squats to 90 degrees or requires assistance (Thomas)
2. 25 squats (to 60 degrees knee flexion) per minute in time with a metronome with a loaded barbell (30% of the participant’s body weight) until the participant falls 4 squats behind or fails at 2 consecutive squats (Frank)
3. 3 single leg squats followed by random jump protocol until 3 squats in a row could not be completed without assistance
When I performed the two protocols, the first took over 20 minutes because the jumps gave me a rest break. The limited motion required of the second was significantly easier and once again took time to cause fatigue. So this is hard to accomplish if the clinic is not set up for it. Our knee group accounts for this by constantly testing motor control along with fatiguing activity throughout training. We now will also separate fatigue with controlled anaerobic exercises followed by 2D biomechanics testing.
The change in motor control is expected with fatigue. Unfortunately, the tendency to develop visual dominance requires central motor planning. Therefore, this reduction in performance may be the result of this central nervous system change as well. It makes me wonder if initiating a disrupting exercise like blindfolded balance, blindfolded step-down, or stroboscopic glasses with cutting and running will break this pattern resulting in improved performance during a fatigued state.
In order to adequately test an athlete that wants to go back to soccer or basketball, a test has to be done under fatigued conditions. If variables like contact noise, limited knee flexion or knee valgus become worse during landing, then this athlete is not ready for play. You can try to make the argument that they are ready, but really it is just going to be a matter of time before they return because of another tear.