We perform running analyses every day.
Viewing your running pattern lets us see you move from one phase of running to the next, from stance to float to swing. There is always something present that would fall out side of what others consider perfect form. Over striding may be present. You may appear to pronate too much. You may be a heel or forefoot striker. We may see that your knees hit together.
But we do not start with a running analysis.
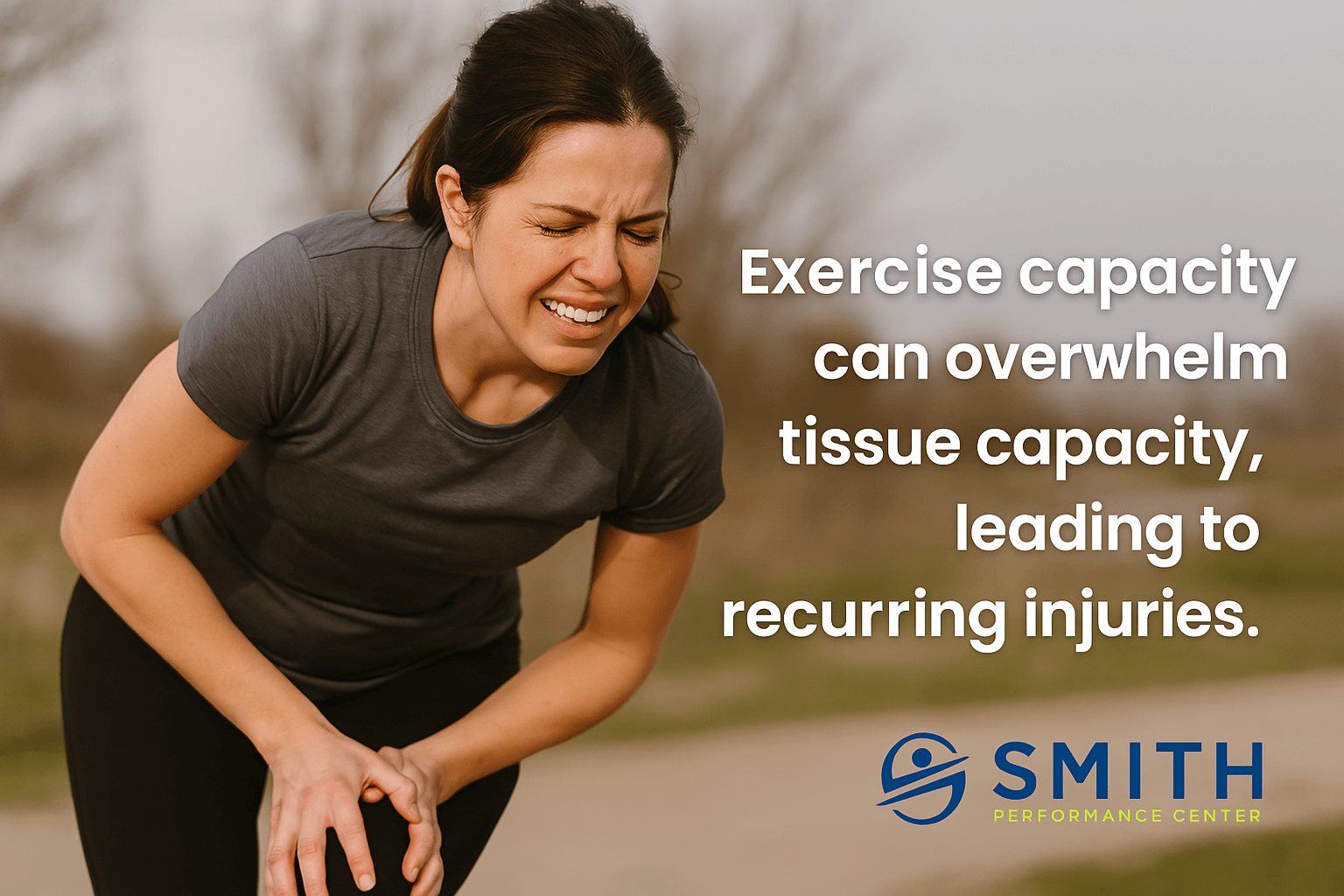
The insights above may get you back to running. However, the truth is that analyzing running gait is not enough. The how and why someone runs with their current pattern or why they keep having an injury cannot be determined by watching them run without checking out the other 5 contributors. Resolving it is not as simple as a switch to a midfoot or forefoot, which is the most common statement we hear from runners looking to run pain-free using a gait change.
You need a solid diagnosis if there is an injury and an examination of the other contributors to your current gait pattern.
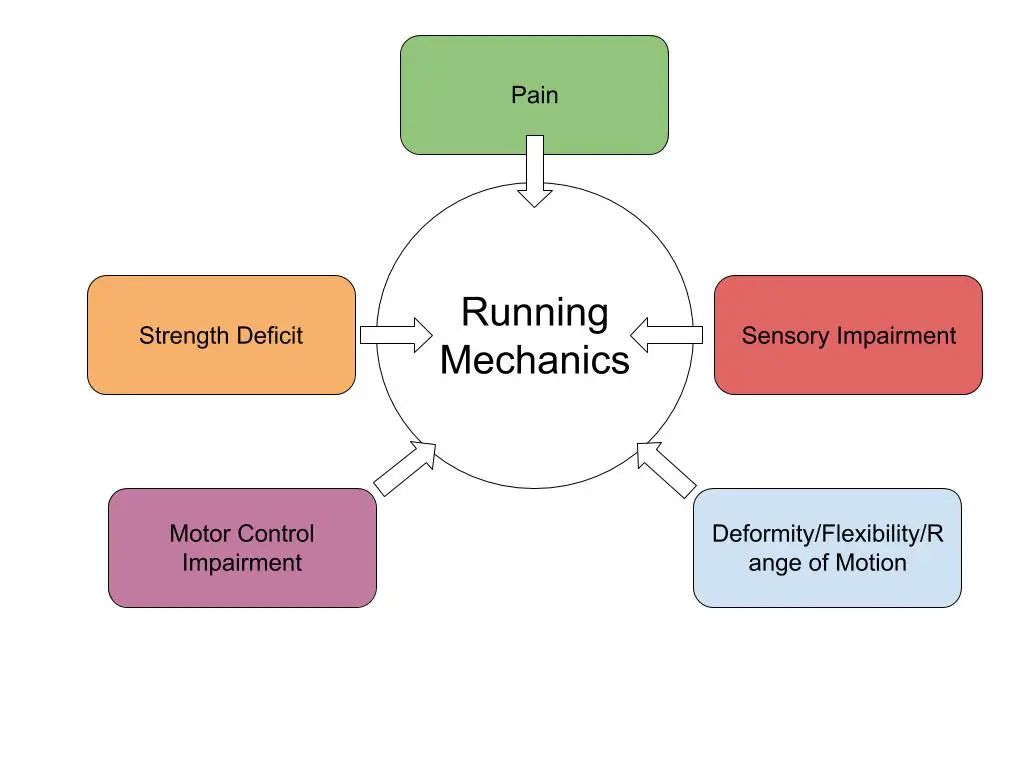
5 Contributors To Your Running Form That You May Be Missing
We have to dig into the exam, which seems to surprise runners that come to see us because we have a reputation as running gait specialists.
Without a thorough exam, your running pattern, also known as gait, cannot be explained. We can determine how much pelvic drop is present or how much you knee flexion you are missing at midstance, but the ‘why’ is missing. The ‘why’ is critical for helping get you past the injury.
Modified from MD, J. P. & PT, J. B. P. Gait Analysis: Normal and Pathological Function. (Slack Incorporated, 2010).
There are 5 contributors to examine:
- Pain
- Deformity/Flexibility Limitations/Passive Range of Motion Loss
- Strength Deficit/Muscle Performance
- Motor Control
- Sensory
Pain
When pain is present, movement changes.
Think of how a person in pain starts to hobble at the end of the race if there knee hurts. While they may be still running and pushing through, the pain will typically not allow their normal pattern to come through. If you have pain when you walk through the door, our number one goal is to understand what the pain generator is (click here if you want to understand our diagnostic process).
The area of pain also matters.
For example with knee pain, we often see a loss of knee flexion angle at mid stance. With pain in the big toe, we see excessive rotation at the hip to avoid toe rocker. The point is that the changes in the gait pattern are not driven by a form problem but a pain problem.
Deformity/Flexibility Limitations/Passive Range of Motion Loss
Humans are amazing at compensation.
A limit in muscle length or at a joint will lead to a change in pattern. Like the example above, we may see the foot turned out if the big toe is stiff instead of painful. Limited ankle range of motion may cause an early heel rise. Loss of hip extension may lead to excessive lumbar extension during trailing limb. What is most critical to understand is that the area during the gait analysis that is abnormal may be driven by some other area.
Without testing, you will not know.
Strength Deficit and Muscle Performance
This is probably the most common problem.
For example, the loss of posterior tibialis strength can lead to rapid pronation that leads to injury and medial ankle overload. The rapid deceleration of the foot and lower leg relies on passive structureswhich is the problem (What is the posterior tibialis and how can you strengthen it?), instead of too much pronation, .
We also see some muscles become weak in common patterns with running.
This includes the calf muscles, the quads, gluteus medius, and gluteus maximus. A true weakness means that activation exercises do not make it better. This requires systematic training of the muscle to get stronger while other become over active such as the hamstrings and TFL. These normal adaptations to running can make your running gait look bizarre. If the gluteus medius is not strong, you will see significant pelvic drop with every stride. I also throw in muscle inhibition in this category. We see runners that test very strongly but after running for 5 minutes, they test weak. This is not fatigue but altered neuromuscular control. We also see cramping where some muscles fire too easily.
Motor Control Impairment
Motor Control is defined as the process of initiating, directing, and performing purposeful voluntary movement.
We can check an individuals motor control with different tests that mimic aspects of running. One example would be a step-down test. Another would be single leg balance. If you cannot balance for more than a few seconds, you will clearly be unstable when running which is a series of single leg balances.
Sensory Impairment
A basic example is a lack of feedback from the foot leading to changes in strike and stance phases-like a foot slap or toe drag leading to falls.
Visual dominance following an injury can also change the system. When we catch a visually dominant runner, we will use eyes closed single leg balance to improve their somatosensory system and reduce visual dominance. The results can be funny and scary as many cannot do it! If you are a trail runner having a lot of falls, this may be your problem.
Why does this matter?
These 5 contributors heavily influence your running mechanics.
If you try to start changing your running gait and one of these contributors is the driver, your gait change will not happen. Instead you will compensate and most likely have an injury develop. However if these have been evaluated, you can make changes at multiple levels targeting the contributors and the actual running pattern that you want to augment.
- Modified from MD, J. P. & PT, J. B. P. Gait Analysis: Normal and Pathological Function. (Slack Incorporated, 2010).