“My butt hurts.”
A significant proportion of my conversations start with this statement. She continued, “ I have regular active release along with dry needling. I stretch my hamstring ALL THE TIME and I still have pain.”
Her frustration was palpable.
“I know I have a tight hamstring and there is scar tissue. But it’s been 8 months.”
She assumes the pain must be the hamstring; we call this the pain generator. The hamstring tendon attaches right where her pain starts. The tightness is over the hamstring muscle belly. She describes the pain in a clear way that implicates the hamstring. She made a convincing argument that the hamstring is the issue and the diagnosis has been repeated by multiple medical providers including a physician and two physical therapists. The location matched. Running increased the pain. Another match. Stretching and manual therapy provided temporary relief.
But 8 months into the problem, the pain remains, limiting her activity and exercise while doing all the right treatment for a hamstring strain.
In her mind, I needed to provide a different treatment for the hamstring to make the pain go away.
Patients , like this woman, face significant challenges due to poorly constructed diagnoses, insufficient testing to confirm these diagnoses, inadequate treatment, and a lack of clear feedback loops. I hate hearing about the months or even years lost doing something they love because of bad strategy. The frustration she felt is due to an unclear process that is difficult for patients to understand, the lack diagnosis testing, and a loss of focus on what problem was being solved (in this case, its what is her pain generator).
Let’s go back to the story.
Why didn’t the hamstring injury improve?
The diagnosis was wrong.
Why did it take 8 months to figure that out?
The previous providers did not use a system to test their assumption that the hamstring was the pain generator. This is a common diagnosis mistake in physical therapy and orthopedics. Any orthopedic problem requires digging into the history and developing a list of differentials (this means different potential pain generators including a chronic hamstring tendinopathy). The first phase of diagnosis requires a thoughtful inspection of the entire history. Snap judgements, uncontrolled biases, and poor heuristics derail the quality thinking needed to make a good diagnosis.
By following a simple series of steps, patients and providers can limit these issues, which we will examine further below.
What do we mean by diagnosis?
The importance of a working hypothesis and differential list
Diagnosis, specifically medical diagnosis, ‘is the process of determining what pathology explains the signs and symptoms a patient exhibits.’
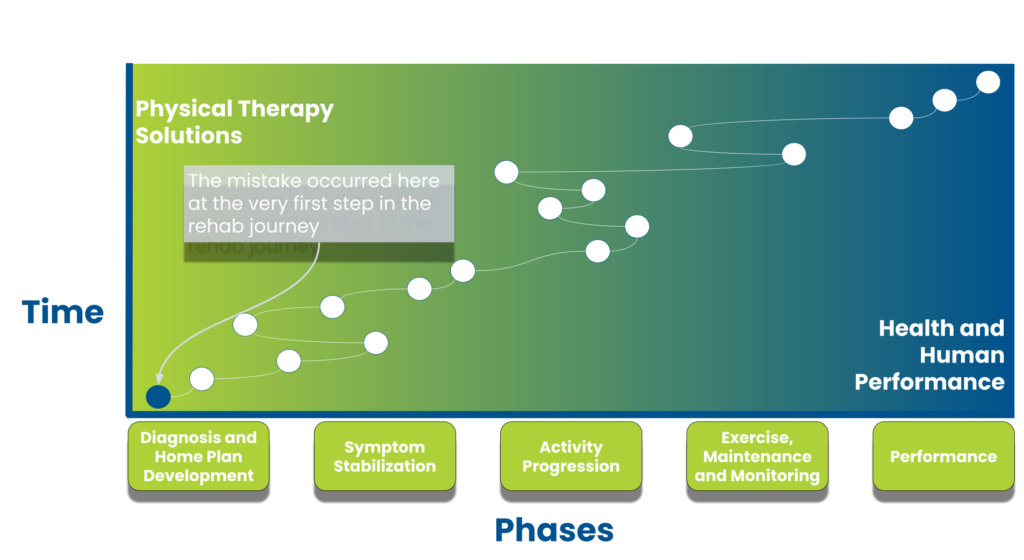
For our team, diagnosis is the first and most critical step of the rehab process. We create a mental model next. Mental models are recurring concepts that are used to improve our interactions and thinking in the real world. The diagnostic process provides numerous steps to mess up. In the example above, the original practitioner only considered one diagnosis then set up a treatment plan without feedback tools. I consider this a profound mistake because orthopedic diagnosis is difficult, prone to biases, and often wrong.
There 3 advantages a physical therapist has in comparison to an orthopedic physician: the frequency of follow-up visits, the time during each visit, and the constrained diagnostic tools.
With the extra time, well timed follow up sessions, and the inability to ‘overtreat’, hypotheses can be tested. Literally, I test and retest up 20 or 30 times when building out my diagnostic conclusions.
The steps are simple.
- What are the possible diagnoses from the subjective?
- What are the possible diagnoses from the objective?
- What is my top diagnosis?
- What is the physical therapy treatment that would most rapidly support the diagnosis?
- Did the treatment result in an improvement in the most painful objective test?
Yes? Continue the same treatment and increase certainty in the top diagnosis
No? Attempt a different treatment for the top diagnosis and repeat steps 4 and 5
After 2-3 rapid treatments without improvement, the next diagnosis and treatment are attempted, repeating steps 3-5. This is part of our key sign and treatment hierarchy process.

How does a diagnosis help in our thought process?
I am regularly wrong on the first diagnosis.
I blunder because I am human and because the body is incredibly complex. I mishear a portion of the story. I ask an unclear question. I do not interpret an exam test correctly. Patients tell me they feel tightness but they actually feel pain. I look at all the questions asked and the exam performed, and none of them make a great picture. I hear a patient say they have pain while sitting. Instead of asking a follow-up question to clarify between two possible diagnoses, I jump to the next question.
There are numerous ways to mess up.
If you understand that diagnosis is complicated and mistake prone, then you never feel confident in your diagnosis. You become the person that constantly questions assumptions, like the assumption that the diagnosis is correct despite treatments that should make the symptoms better, are not. Diagnosis becomes a process within every physical therapy session instead of one time thing done at the start of a plan of care. With all that can go wrong, it is a profound mistake to limit the differential diagnosis list to one pathology that you do not confirm. This is compounded when applying the same treatment over and over again without useful tests to show progress.
Using the following steps with a clear home plan sharpens the diagnosis until your differential list becomes one with the highest probability of explaining all the information you collected.
Steps in Diagnosis at Physical Therapy
Step 1: What are the possible diagnoses from the subjective?
I started questioning how the pain started, when it is felt, and how much.
What is the quality of the pain? Does she feel it when the leg is swinging through while walking? Is sitting the most problematic issue? What is she leaning back while sitting? The questions irritated her at first. In her mind, she had a hamstring tendinopathy, but the questions started to shift the probabilities.
I finished the interview and my differential list included the hamstring, but I put it as the lowest probability diagnosis.
Top 3 Differentials:
- Discogenic low back with somatic referral
- SI joint Lesion
- Hamstring Tendinopathy
Step 2: What are the possible diagnoses from the objective?
I tested the back, SI joint, hip, and hamstring.
I recreated her buttock pain with a slump test, indicating neural tension, and active back motions. I did a posterior to anterior pressure on her L4 and L5 spinous process that recreated the buttock pain as well. The probability of the low back causing the pain went much higher. I resisted the hamstring muscle – no pain. I stress the SI joint – no pain.
Top Differentials:
- L5-S1 Discogenic low back with somatic referral
- L4-5 Discogenic low back pain with somatic referral
- Clinical Lumbar Instability
Step 3: What is my top diagnosis?
At this point, I felt 90% certain that the injury was originating from her low back.
I was not sure which level was most responsible for the pain, but I could provide treatment at this point to confirm.
Step 4: What is the treatment that would most rapidly support the diagnosis?
I decided to start with gentle lumbar traction.
Since my top diagnosis is the lumbar spine, this will target the back. There is a fast feedback loop as I can traction for a brief period of time and retest for any change.
Step 5: Did the treatment result in an improvement in the most painful objective test?
I tractioned her low back and her pain in the buttock reduced with retesting of the painful exam.
By the end of the visit, her buttock pain was 80% reduced with sitting. I adjusted her home plan to stop hamstring stretching and to lie down 2-3 times per day for 10 -15 min. At the second visit, she no longer had pain unless she sat for over 2 straight hours. We made sure she sat no longer than an hour forty-five.
The home plan was based on her actual pain generator and activities should could do on her own to make it better.
Diagnosis matters and needs to be part of the rehab process
Diagnosis is complicated.
The problem requires interviewing, testing, assumptions, and feedback in a big loop. In the example, the butt pain mimicked a hamstring injury. The treatment for 8 months never targeted the actual injury. If you hear a clinician say, I know exactly what that is after a few seconds of conversation, you should be worried. All clinicians develop biases in their practice and use heuristics, rule of thumb, to make decisions. Without a system, diagnosis is a crapshoot with terrible results.
As a patient you can ask and use steps above to help with your treatment.