Prognosis and Outcomes in Physical Therapy
One of the key differences in our practice compared to normal, insurance-based physical therapy is how we schedule our sessions. We normally do a session once every week or two weeks. This developed as a result of our focus on the home plan including trigger management. The second reason was how we started to use braces, tape, and training aids.
How do the anatomy and function of the rotator cuff impact physical therapy?
What is my rotator cuff injury?
How long till my rotator cuff injury is better?
Prognosis with a Rotator Cuff Injury
In the first two parts of this series, we looked at the background information about the structure and function of the rotator cuff, the common types of Rotator Cuff injuries that lead to pain, and how to figure out what it is. With this final article, we would like to offer some perspective on how rotator cuff injuries typically resolve.
Rotator cuff injuries have a wide range of outcomes, but most can be treated successfully.
If we catch symptoms in the early stages of tendinitis, this is a quick fix that only takes 1-2 visits.
If symptoms have been allowed to progress, we may have to spend more time changing movement patterns and modifying daily activities to allow for healing. A mid-range prognosis is typically about 4 visits.
If symptoms have progressed to the point of partial or full-thickness tearing of the rotator cuff, the prognosis is highly variable. The prognosis will depend on the extent of the tearing, a patient’s current and target activity level, the amount of pain they are experiencing, and whether or not there are any other accompanying injuries.
Anecdotally, we have seen patients diagnosed with full-thickness tears of one or more rotator cuff muscles. Some of these patients still play golf or tennis and have an almost full range of motion in the affected shoulder. Their only complaint is pain or weakness in a specific position. This goes to show the variable nature of rotator cuff injuries.
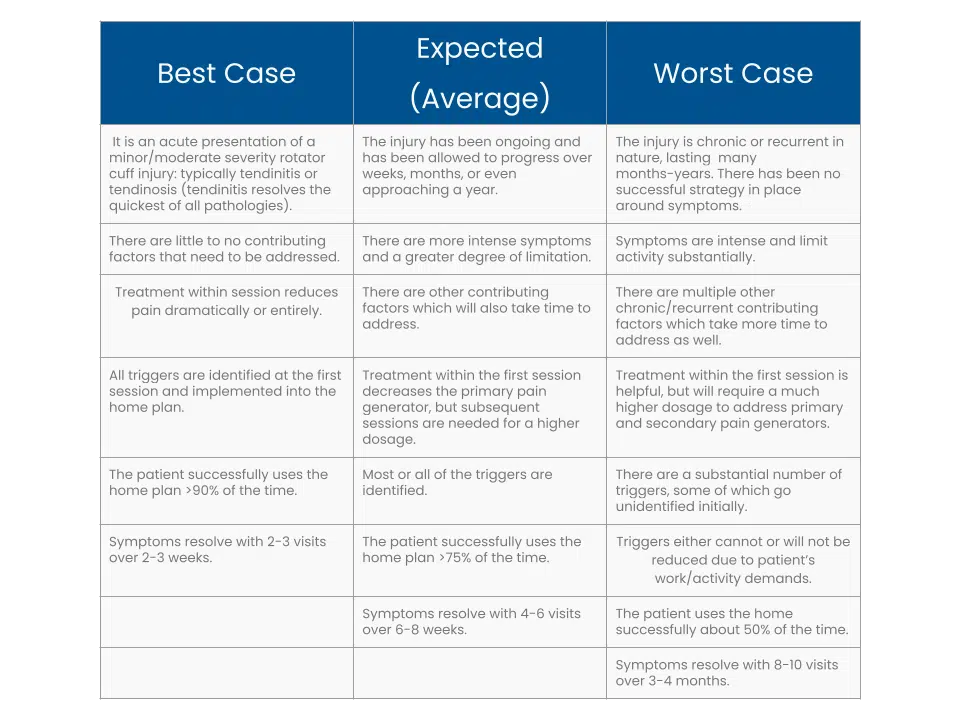
Rotator Cuff Outcomes
We view all our outcomes using a three-tiered system, or a three-level prognosis (read about how this informs our practice). For rotator cuff injuries, this breaks down as follows:
Conclusion: other considerations regarding shoulder pain
While this series of articles provides a comprehensive look at the rotator cuff from subjective complaints to outcomes, there are many other considerations that go into managing rotator cuff injuries.
If the initial diagnosis and treatment are off or do not have the typical response, the clinician must work back through the exam and consider other differentials.
Oftentimes there is dysfunction along the kinetic chain, starting with the thoracic spine, ribs, and scapula which also needs to be addressed.
Instability is another common finding which contributes to rotator cuff injury and requires further modifications to the plan.
Managing rotator cuff injuries does not have to be a grueling process for the patient and clinician. With a clear plan in place, most cases tend to follow the best-case scenario in the three-level prognosis.