Why is your heel pain not getting better?
Heel pain is a common, painful foot condition leading internet searches for “cures to heel pain” or “treatments for plantar fasciitis.”
The pain resolves with time if the cause of symptoms is removed, but up to 10% of individuals with heel pain do not get better. These chronic sufferers try everything to get rid of the pain including plantar fascia releases, injections, and pain medications. The causes of heel pain are numerous, ranging from plantar tendinopathies like the flexor digitorum brevis, nerve involvement with tarsal tunnel syndromes or lateral plantar nerve, low back referrals, and double crush syndrome to fat pad injuries. The answer is not more stretching and new orthotics.
If you are stuck with heel pain and the typical treatment for plantar fasciitis is not making you feel better, then you likely have a different problem and require a different approach.
4 ways to reduce your heel pain
There are 4 ways to start feeling better:
- Target the correct pain generator (read 7 Signs Your Heel Pain Is Not Coming From Your Plantar Fascia)
- Quit irritating the pain generator on accident
- Absorb load better
- Use artificial stabilization or support
Understand what tissue is causing the pain
Plantar heel pain can be caused by the Flexor Digitorum Brevis, Abductor Hallucis, Abductor Digiti Minimi, Fat Pad Trauma or Atrophy, Calcaneal stress fracture, Lateral Plantar Nerve, Medial Plantar Nerve, Tarsal Tunnel Syndrome, low back referral, hip joint referral, Plantar Fascia, and surgical scars.
That may seem like a long list, but each of these has been seen clinically at our office. If your heel pain is not getting better, the first step is determining the pain generator. This is called a diagnosis and it can be very difficult even for a trained professional. I realize you are wondering how to do that on your own. I use a series of questions that you can ask yourself.
Question #1
Is there cramping on the bottom of your foot that causes the pain? If you answer yes to this question, then it is a muscle and most likely the Flexor Digitorum Brevis, Abductor Hallucis, or Abductor Digiti Minimi.
Question #2
Is there burning, numbness, or tingling? If you have any of these symptoms, then you have some type of nerve involvement which could include Lateral Plantar Nerve, Medial Plantar Nerve, Tarsal Tunnel Syndrome, or Low back referral.
Question #3
Is the pain severe, well-defined, and located directly on the bottom of the heel? This means you may have hurt the fat pad. This can get better but you need to stop loading the heel.
Question #4
Does your pain seem diffuse or hard to describe with a location that can change? This is typical in referrals from other areas of the body. Since the foot has a dense receptor field, your inability to precisely and clearly locate the pain means it could be coming from the low back or hip.
If you have been told that you have plantar fasciitis, and you answered yes to the first question, read our post ‘7 Signs Your Heel Pain Is Not Coming From Your Plantar Fascia.’
Quit irritating the pain generator on accident
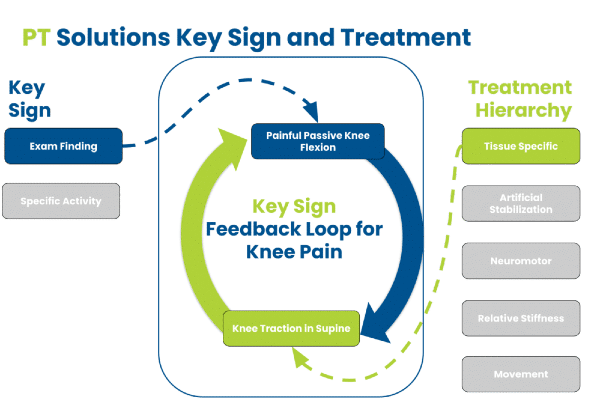
Once you have an understanding of the pain generator, the next step is to understand what makes it worse.
Our team calls this trigger management. It is a borderline obsession for us. There are clear triggers for each of the different pain generators. Unfortunately, the triggers are not the same for each tissue. There are a few common triggers to check out and make sure they are not part of your problem.
Stop burying your toes
If your main problem is the flexor digitorum brevis, then we look at the footbed or insole.
The insole shows how you use your toes inside the shoe. If you see that the insole has clear holes or deeply worn-out spots where the toes touch down. This means you are burying your toes. The original cause of this is not clear but is a difficult trigger to get rid of because you do it without knowing.
The easiest way to start is an exercise we call toe walks.
Neural tension
Neural tension is an issue we see with spine injuries and nerve injuries.
A nerve is mechanically sensitive to stretch with chemical sensitization. Any time you have an injury, there is a chemistry that gets thrown out that the nerve finds irritating. This irritation leads to an intolerance of stretching the nerve. If your heel is feeling numb, burning, tingling, or even overly tight, you may be stretching a nerve.
If you are doing this, the injury will not heal.
Cramping
If you have cramping, then it’s time to wage war on what is causing it. The plantar intrinsic muscles will be predisposed to cramping if you put your foot and toes into a plantar flexed position.
Here is a quick list of potential culprits:
- Lying on your back with the sheets tucked into the mattress
- Swimming with fins
- Sitting with the feet tucked backward
- Rear Elevated Split Squats with the top of the foot on the bench
- Quad stretching in standing with your hand grabbing the top of the ankle
- Pressing the toes down into the ground, inducing a cramp
There are activities that interact with each other and lead to cramping/and or increased pain:
- Swimming followed by biking (The number one issue with triathlete training)
- Running following sitting with the foot plantar flexed
- Sitting with the feet and toes plantar flexed followed by walking
Constant heel load
If your fat pad is injured, you are likely loading it all of the time.
The fat pad absorbs force and is incredibly good at it. If you damage it or there is loss of the fat pad, call fat pad atrophy, then the underlying bone can become very painful. If you stand all day, then it is almost impossible to make the heel better. You must unload it.
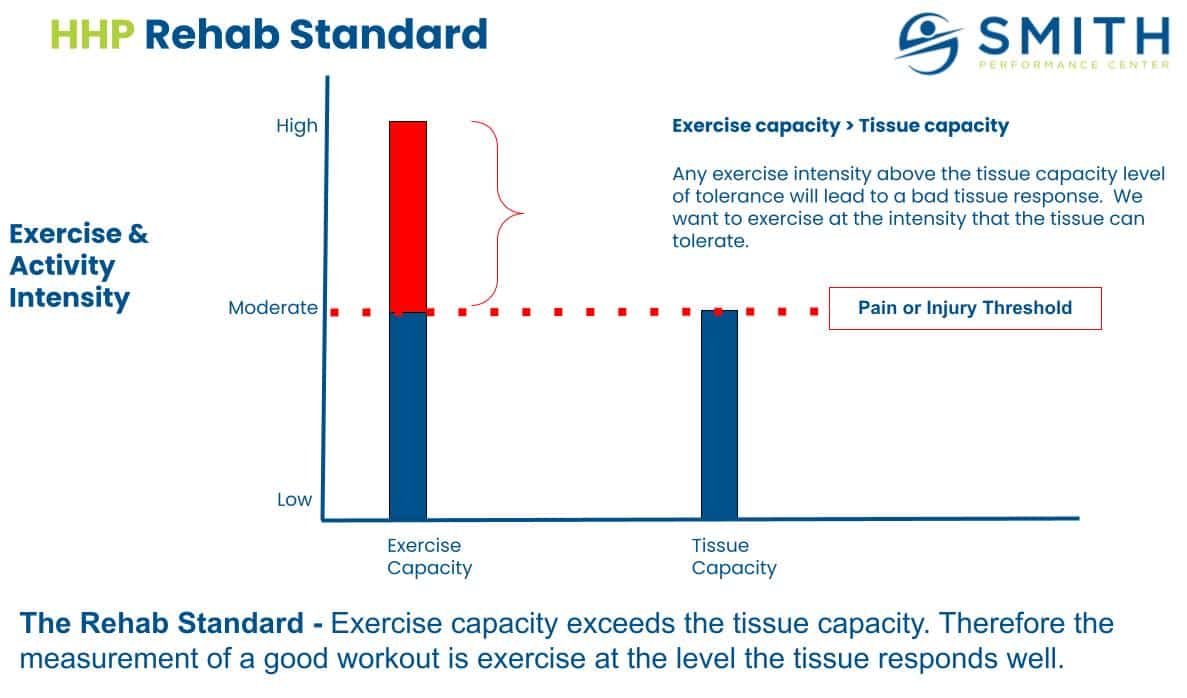
Absorb load better
The lower leg is meant to absorb force.
Every step you take will load the muscles and ligaments. Humans do it so well that we can do it without thought. The force absorbers of the leg can become inhibited (shut off due to pain or some other cause) and/or weak. When this happens, the tissues around the heel can get overloaded. The performance of the leg muscles can be improved by doing activation exercises for the following muscles: Posterior tibialis, Anterior tibialis, Flexor Hallucis Longus, Quadriceps, Gluteus Medius, and Gluteus Maximus.
If each of these muscles functions better then heel tissues will not be overloaded, allowing it to heal.
A great place to start is with the glute activation while keeping the heel unloaded.
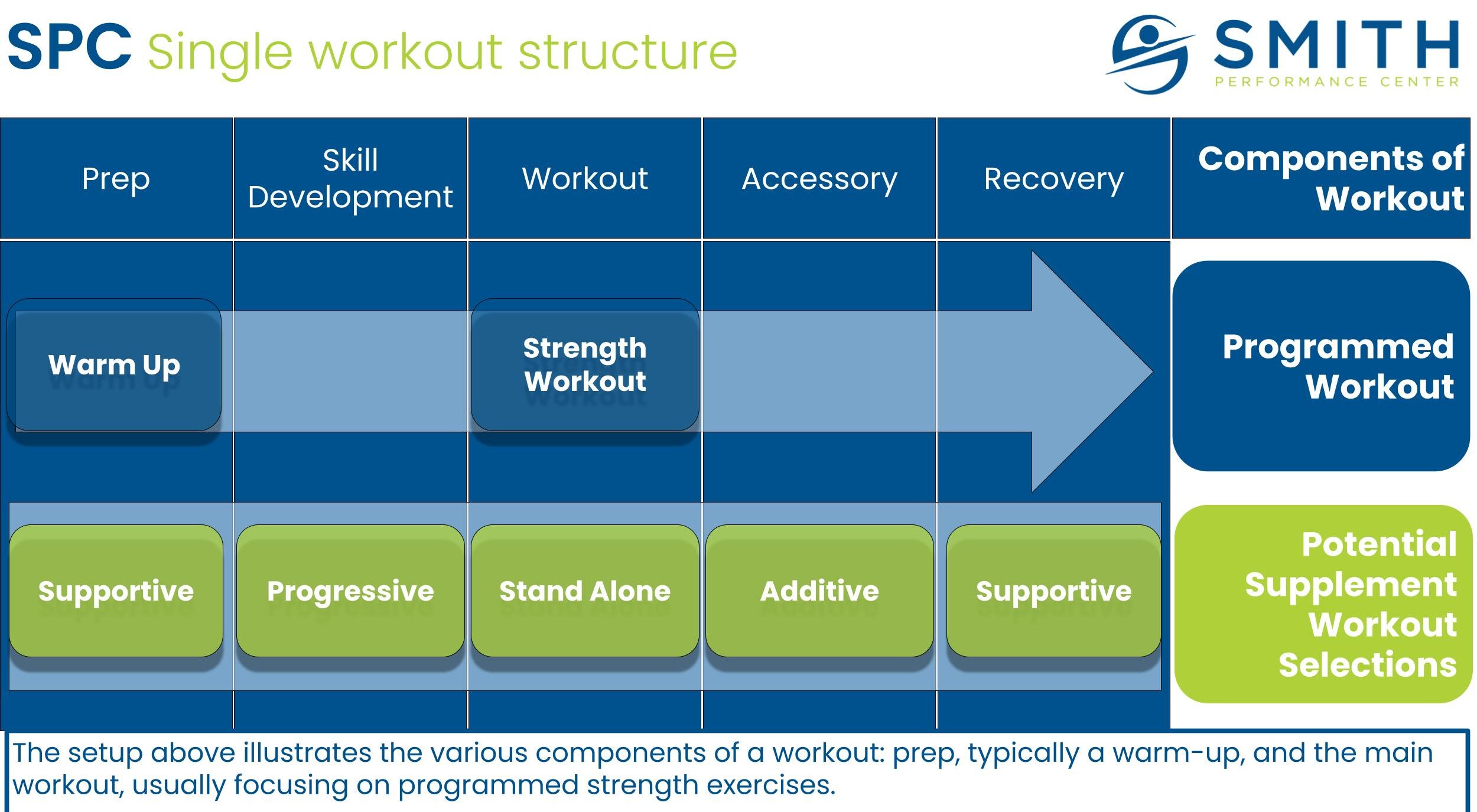
Use artificial stabilization or support
There are numerous bracing, taping, and support tools available to those with heel pain.
Often I see patients default to expensive and permanent orthotics for an injury that does not require it. Artificial stabilization helps to improve force absorption and reduce load. The easiest way to understand what to use is to look at when you feel the pain with walking then use artificial stabilization to help the normalize the loads in the foot. This can be more easily explained by the functional rockers in the ankle and foot during the gait cycle.
There are three very useful tools that you can try to use: modified low dye, posterior tib brace, and heel protector.