How to Avoid “Exercise Hell” (When Exercise Makes You Feel Worse)
When exercise makes you feel worse instead of better, motivation isn’t the problem. Learn why this happens and how to avoid “exercise hell.”
Find related articles and learn more about our process at SPC.
When exercise makes you feel worse instead of better, motivation isn’t the problem. Learn why this happens and how to avoid “exercise hell.”

Why injuries keep coming back after the first one. Learn how tissue capacity, compensation, and the therapeutic gap lead to recurrent injury.
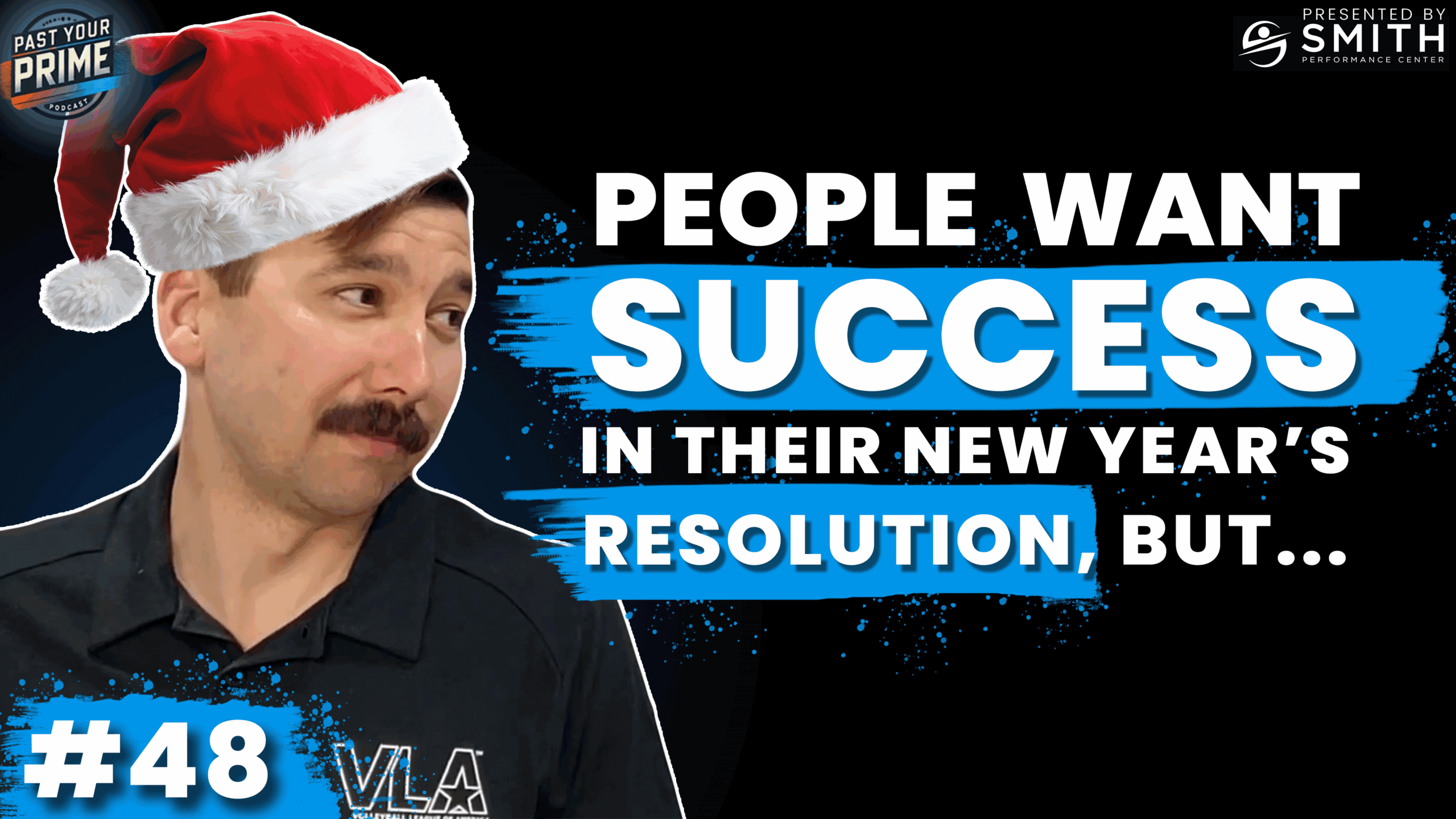
Stretching is supposed to make your hamstrings feel better—looser, lighter, more flexible. So why are you experiencing only temporary relief at best—and often feel even more sore after stretching? There’s a deep cultural belief in the power of stretching to reduce pain, improve mobility, and prevent injury. The support for those claims is, at best, inconsistent or non-existent. 1,2 If you’ve found this article, you’ve likely noticed a pattern yourself: every time you stretch your hamstrings, they get worse. At Smith Performance Center, we see this pattern constantly. The sensation of “tight” hamstrings is rarely about flexibility—even in those with limited motion. We hear people complain of tightness in tissue disorders that actually cause more motion than normal. More often, it’s a protective signal that something is off in how your system is moving, processing information, or managing load. In this article, we’ll walk through what actually causes post-stretching soreness
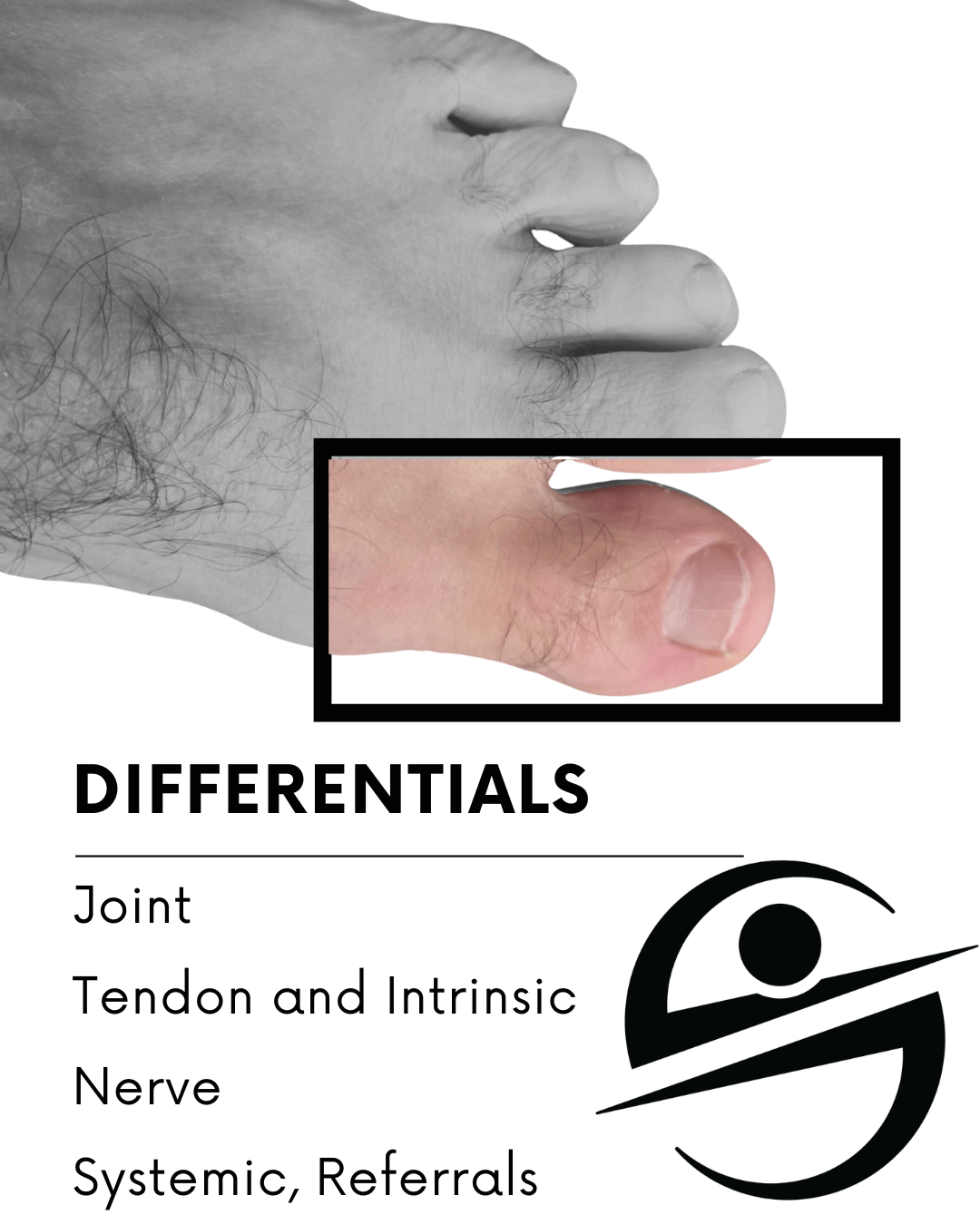
Case Study: The Dancer With Recurrent Big Toe Pain A former college dancer came into the clinic frustrated. She’d stopped dancing years ago, but every time she returned to even basic classes, her big-toe pain spiked. She tolerated hiking in her stiff boots, a little pain but nothing that stopped her — yet one night of dancing, and she’d hobble for a week with a throbbing big toe. Her frustration was visible, and the best advice she’d heard—stop dancing—wasn’t one she wanted to follow. Her last visit with a podiatrist ended with an injection that helped for about a week before the pain returned. She started to believe her big toe would never handle the way she moved in college. There didn’t seem to be a path forward. Her experience—the fake improvement with time off, followed by a big flare when she tries to get back to what she loves—mirrors

Learn how Smith Performance Center helps people with osteoporosis and lifting programs that build stronger bones safely through progressive strength and impact training in Tucson.
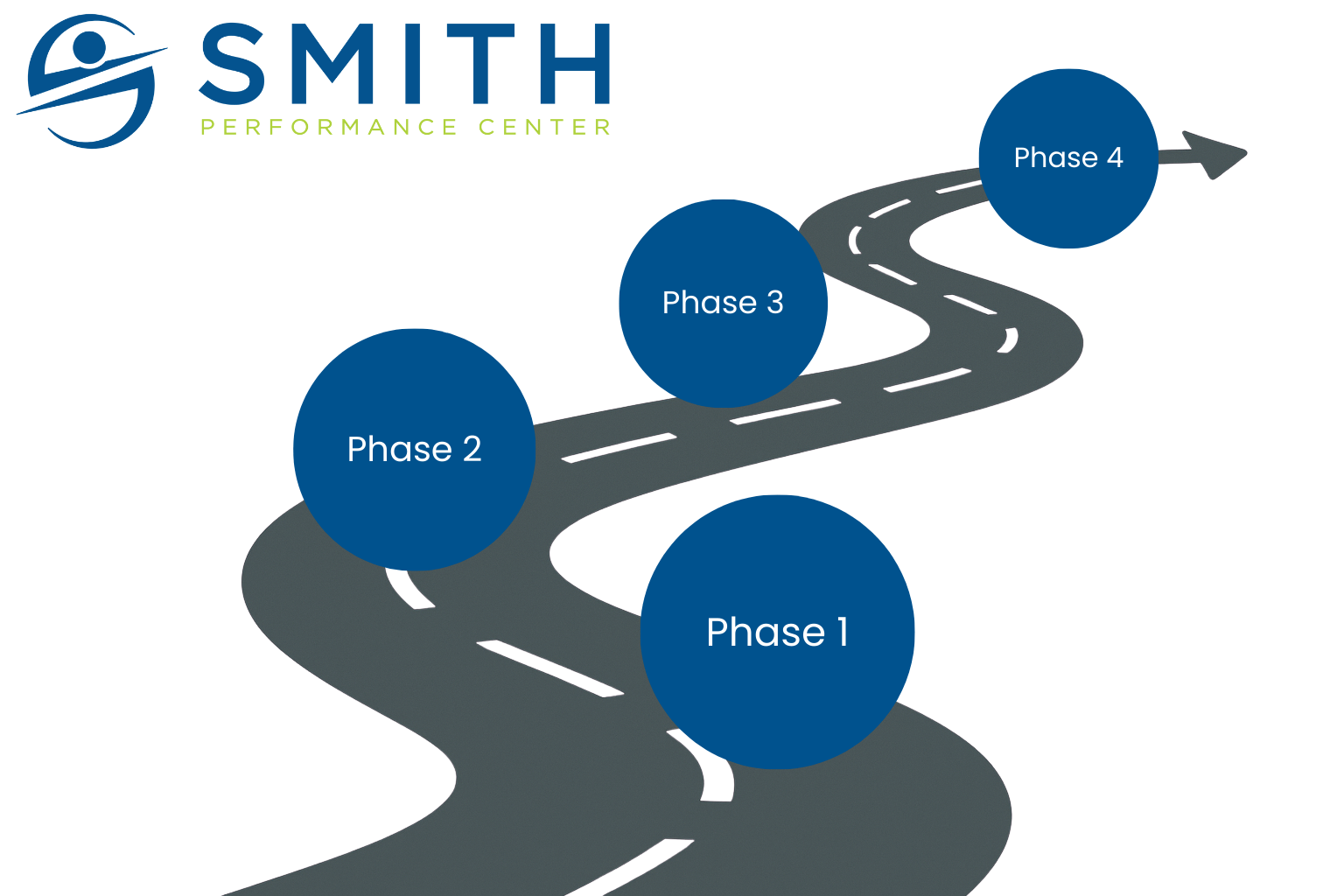
At Smith Performance Center, the home plan is a central feature of your rehabilitation experience. If you’ve worked with physical therapy in the past, you’ve probably been given a list of exercises to do on your own, most often called a ther-ex list or home exercise plan. Our approach is different. The purpose of your home plan isn’t just to give you something to do between visits — it’s to improve your tissue capacity and help you progress safely toward your goals. And the strategy often changes as you move from Phase 1, where we identify and outline what is causing your pain, to Phase 2, where you learn to manage your symptoms, to Phase 3, where we work to build your tissue capacity and progress your activity. Learn more about this process in our article “What are the phases at Smith Performance Center?“ Why the Home Plan Matters To
You have chronic hamstring tightness. You don’t even remember when it started. So you stretch. You foam roll. You warm up, cool down, and maybe even do yoga. Then you try massage or physical therapy. Maybe you’re told your glutes are weak and you’re handed a list of exercises to fix the problem. And yet, months—or years—later, your hamstrings still feel tight. Sometimes they even hurt. Eventually, you just decide this is probably your life. So you Google it. What Google Says About Chronic Hamstring Tightness “Tight hamstrings are a common issue, often caused by prolonged sitting, intense physical activity, or muscle imbalances. To address this, regular stretching—especially dynamic stretches before activity and static stretches afterward—can be beneficial. Strengthening in a lengthened position can also help. If tightness persists, consult a physical therapist or try massage or manual therapy.” —Google AI + Verywell Health And you think to yourself: “I

If you are trying to find the cause of pain that keeps returning, you are not alone. Many people are given quick labels like tendonitis or a pinched nerve and told to rest but that often does not solve the real issue. At Smith Performance Center, we go deeper than a label. We use a system called the 4 Pillars of Diagnosis to understand the real problem and build a clear path to recovery. Each pillar gives us critical information about what is causing your symptoms, how your body is functioning, what helps, and what triggers setbacks. It is the difference between a guess and a plan that works. 1. Structural Diagnosis: What Might Be Injured? This is the traditional starting point in most evaluations. We identify what structure might be involved—whether it is a tendon, joint, ligament, nerve, or muscle. We use hands-on testing, functional movements, and your medical

During recovery, there comes a pivotal moment when symptoms improve, and the client feels like they’ve turned a corner. Life feels good again, and naturally, activity levels increase. This change is often unconscious or unintentional—but its consequences can be significant. A rehabilitation flare-up is defined as a return or increase in the original symptoms that led the patient to seek care. The natural reaction to a flare-up is often to question whether the real problem is being addressed. Read: the diagnosis is wrong. But this reaction can lead to a critical misstep—focusing on the wrong issue and missing an opportunity for patient empowerment. Diagnostic Errors vs. Rehabilitation Flare-Up Mismanagement Achieving the correct diagnosis involves identifying potential tissue pain generators, noting local and regional contributors, considering central modulation, and uncovering triggers. This process requires careful collection, analysis, and prediction. And there can be many reasons that diagnosis is hard, but once
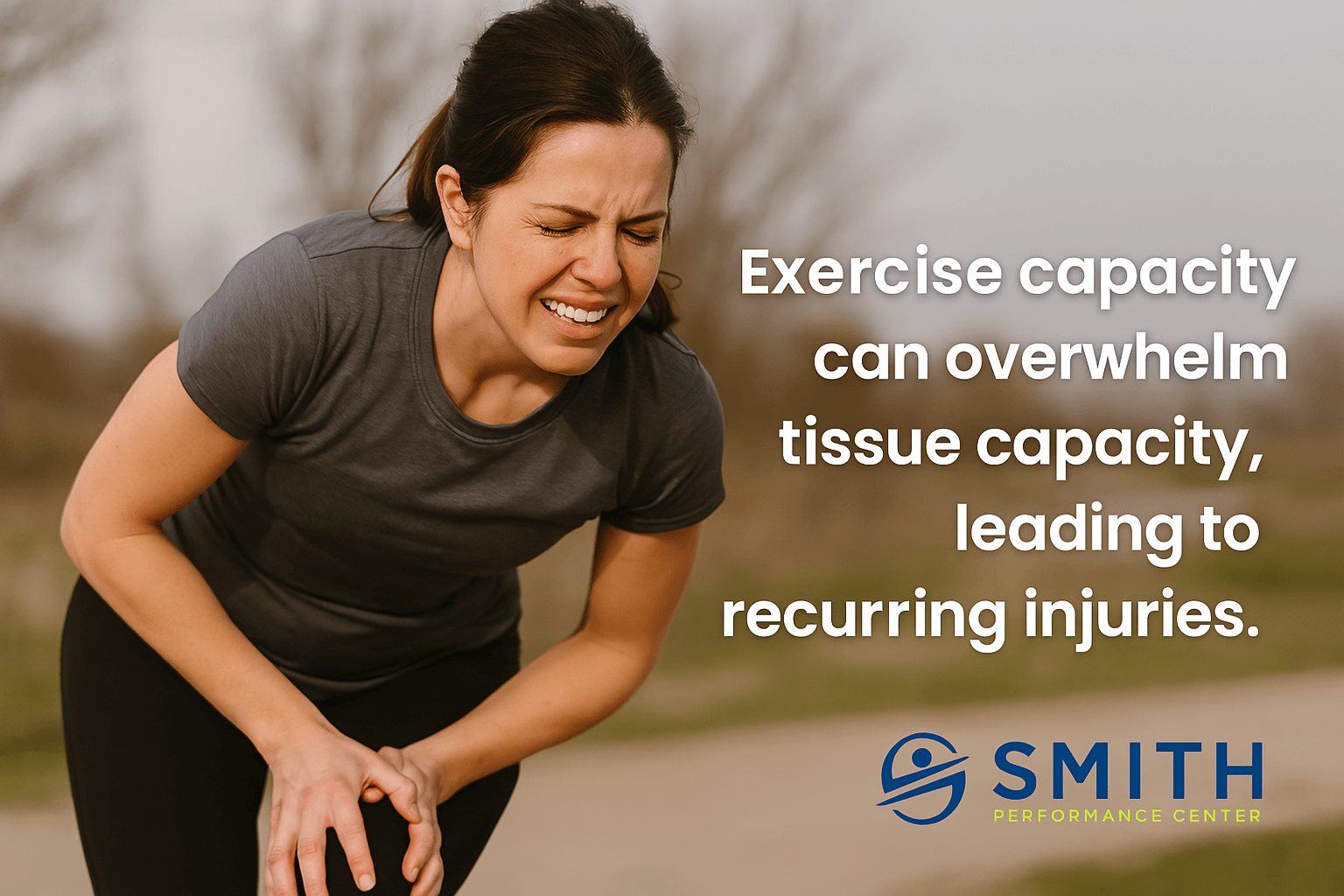
You’re Doing the Work—So Why Does Your Body Keep Breaking Down? You show up. You put in the effort. Whether it’s running, lifting, group fitness, or weekend hikes, you’re trying to stay active. But despite the commitment, you keep dealing with recurring injury from exercise. Pain shows up, progress stalls, and your body feels more unpredictable than it should. This isn’t about motivation. It’s about biology.The real issue is a mismatch between what you can make yourself do and what your body is built to tolerate. At Smith Performance Center, we call that gap the difference between exercise capacity and tissue capacity the rehab standard—and it’s one of the most overlooked problems in rehab and training. What Is Exercise Capacity? Exercise capacity is your ability to push through effort and accumulate work over time. It’s what most people think of as “fitness.” It includes: Exercise capacity reflects what you’re capable