Why Your Hamstrings Hurt After Stretching (and What’s Really Going On)
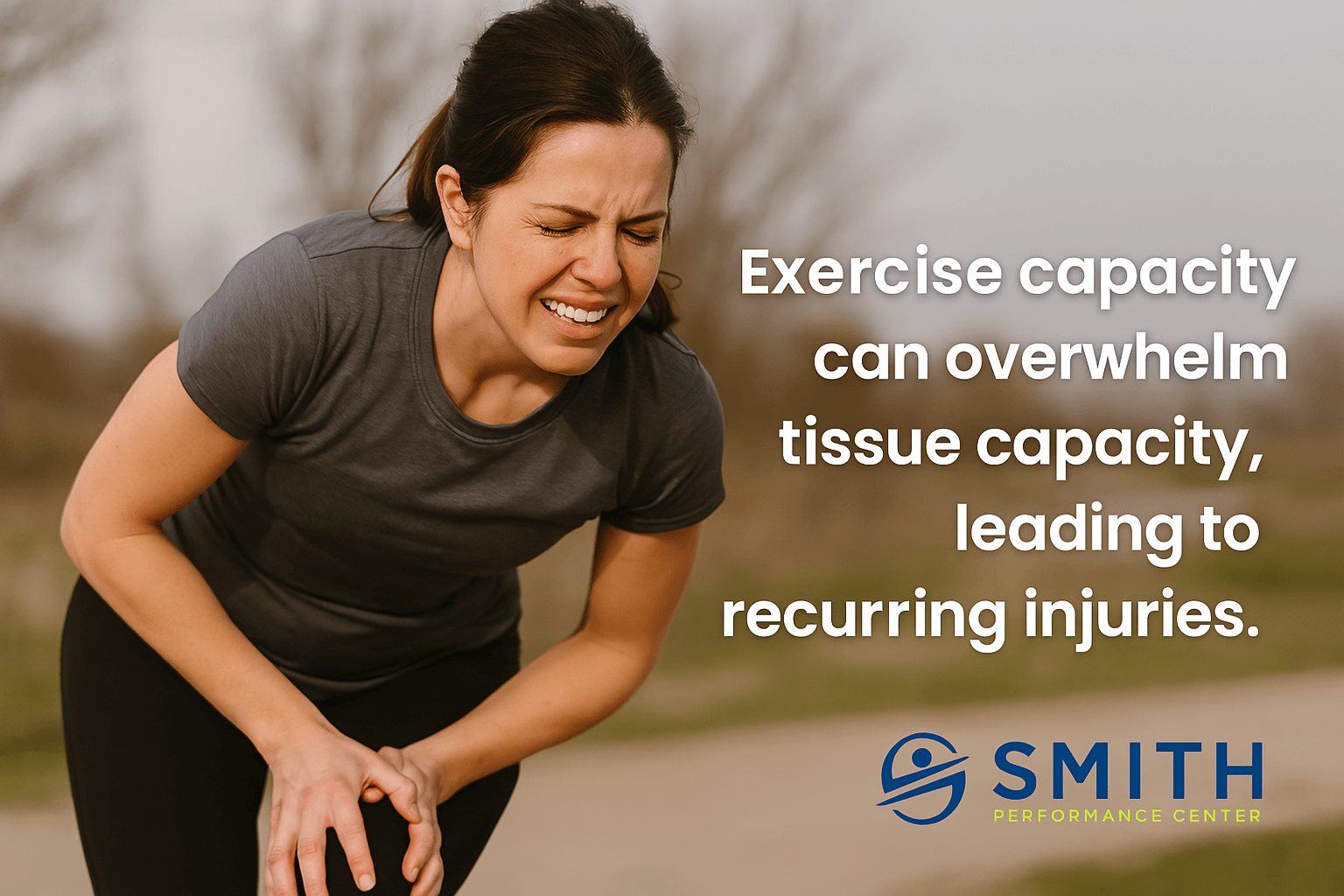
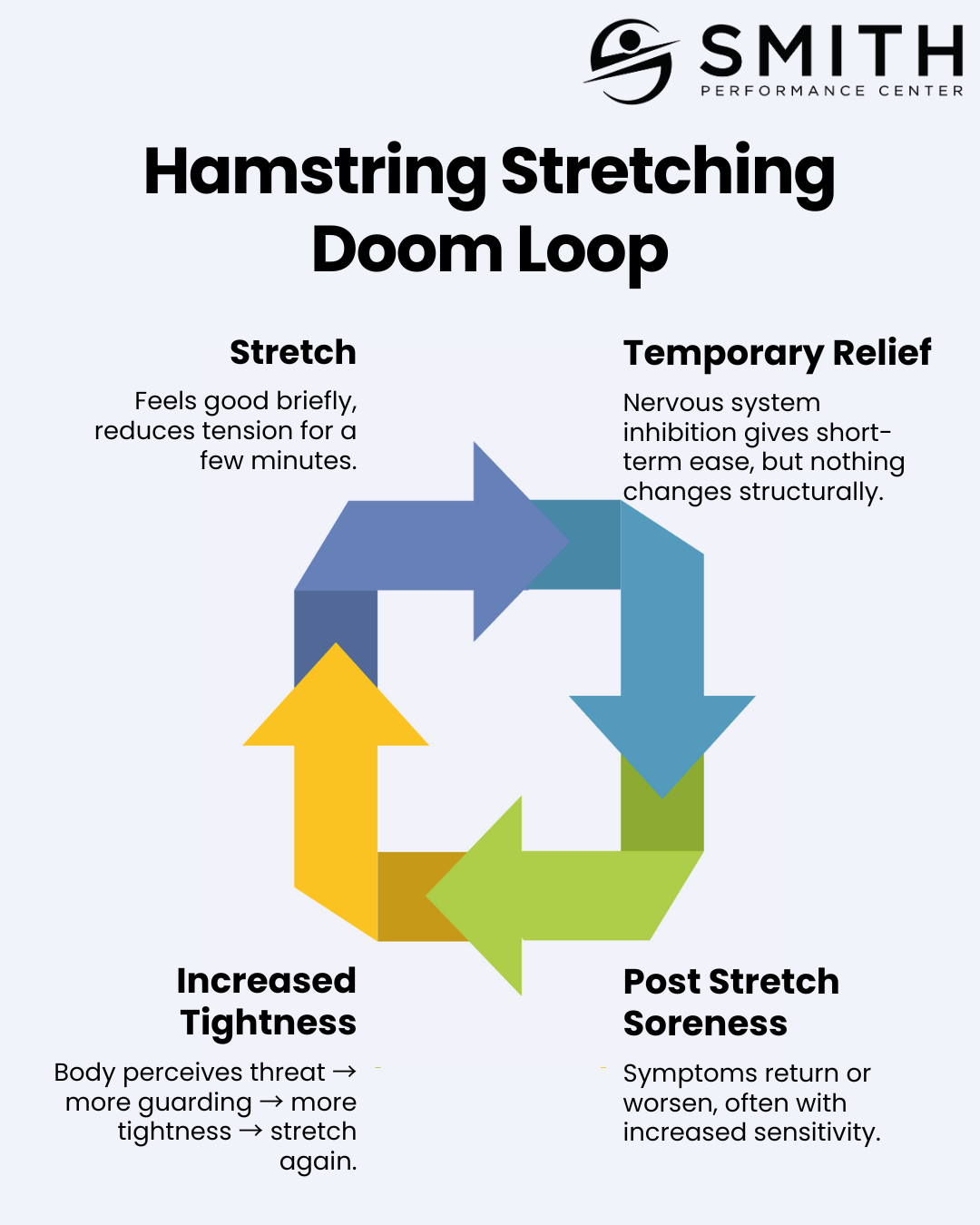
Stretching is supposed to make your hamstrings feel better—looser, lighter, more flexible. So why are you experiencing only temporary relief at best—and often feel even more sore after stretching? There’s a deep cultural belief in the power of stretching to reduce pain, improve mobility, and prevent injury. The support for those claims is, at best, inconsistent or non-existent. 1,2 If you’ve found this article, you’ve likely noticed a pattern yourself: every time you stretch your hamstrings, they get worse. At Smith Performance Center, we see this pattern constantly. The sensation of “tight” hamstrings is rarely about flexibility—even in those with limited motion. We hear people complain of tightness in tissue disorders that actually cause more motion than normal. More often, it’s a protective signal that something is off in how your system is moving, processing information, or managing load. In this article, we’ll walk through what actually causes post-stretching soreness