Total Knee Case Study: Why You Need A Structured Rehab Process
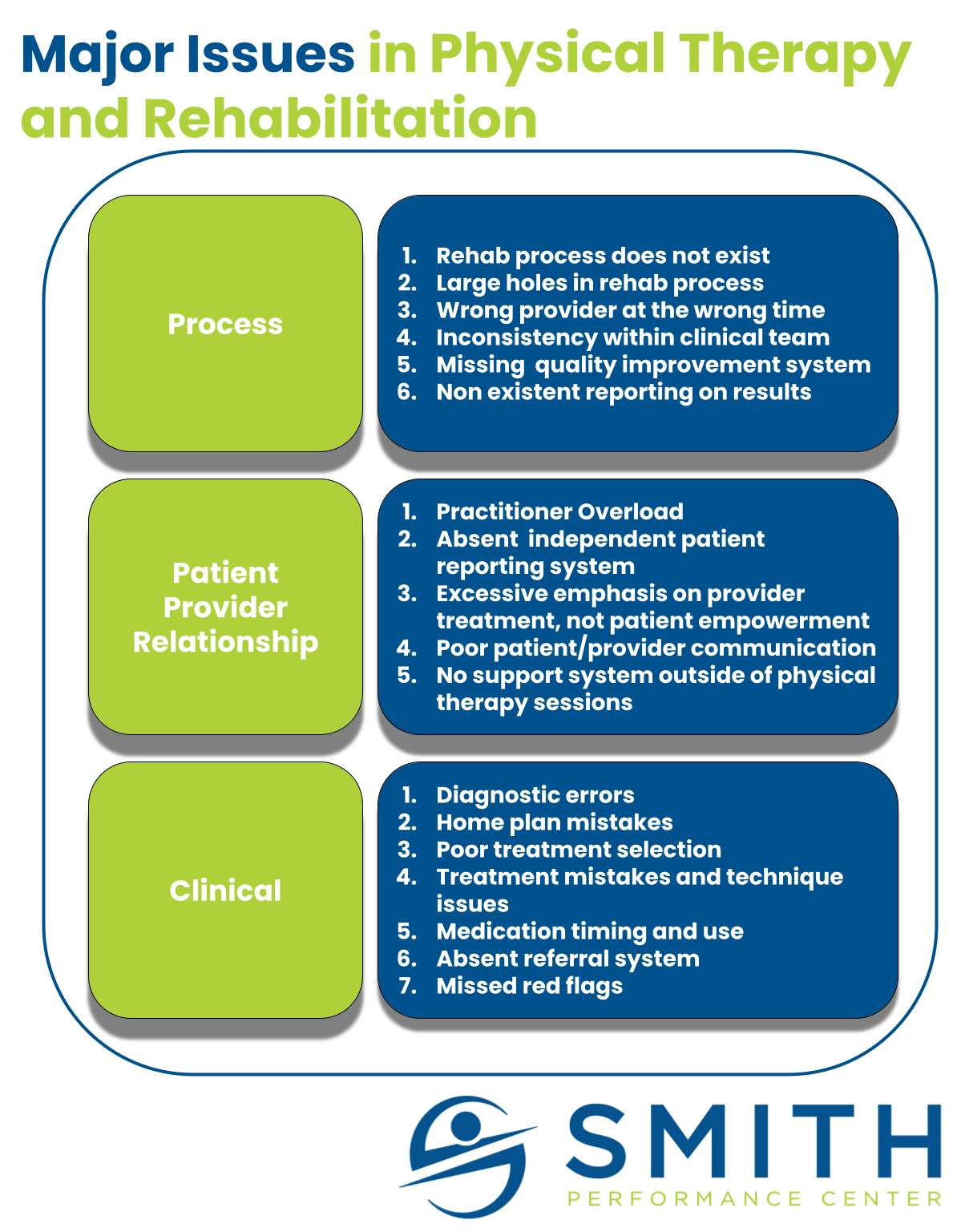
A structured rehab process that ultimately targets a full return to activity is missing in healthcare. Patients struggling with pain are treated as if they are all the same. We believe there are common, big problems to address, but there is a high degree of uncertainty with every patient presentation. Even when a patient has the same diagnosis they can have different triggers, different contributing factors, different behaviors, and drastically different needs in the rehab process. This is true when patients have the same surgery by the same surgeon. Let me use an example with a straightforward rehab plan; post-total knee replacement. The Painful Total Knee Replacement Peter Pain had a total knee replacement. He has always been active and handles pain well but this replacement has been horrible. First, he fell behind on medication post-surgery because he hated the way the drugs made his stomach feel. The second day